Scientists from the Skolovo Institute of Science and Technology (Skoltech) have developed a novel method of 3D printing personalized ceramic bone implants.
Within their research, the team deployed a simulation-based approach to create flexible, flaw-free 3D models that would provide a basis for their additive implants. The researchers’ optimized these designs to feature large pores, that could be customized to suit the needs of specific patients, and make them easier to fuse with organic tissue.
“Functional representation (FRep) modelling of microstructures has a wealth of advantages,” said Evgenii Maltsev, one of the paper’s co-authors. “FRep always guarantees that the resulting model is correct, as opposed to the traditional polygonal representation in CAD systems, where models are likely to have cracks or disjointed facets.”
Harnessing the potential of ceramics
Ceramics possess a number of properties such as wear-resistance and chemical stability, that make them ideal for 3D printing anything from tools to dental products. Despite this, while additive manufacturing has also been adopted within implant applications, ceramics are used less often in this area with cell laden polymers and alloys usually preferred.
Researchers at TU Delft, for instance, have developed magnesium-based regenerative scaffolds, while a Charité–Universitätsmedizin Berlin study found that Titanium was the optimal material base. Elsewhere, Japanese scientists from Nagasaki University and Saga University, have created a 3D tubular trachea structure with no biological scaffolds at all.
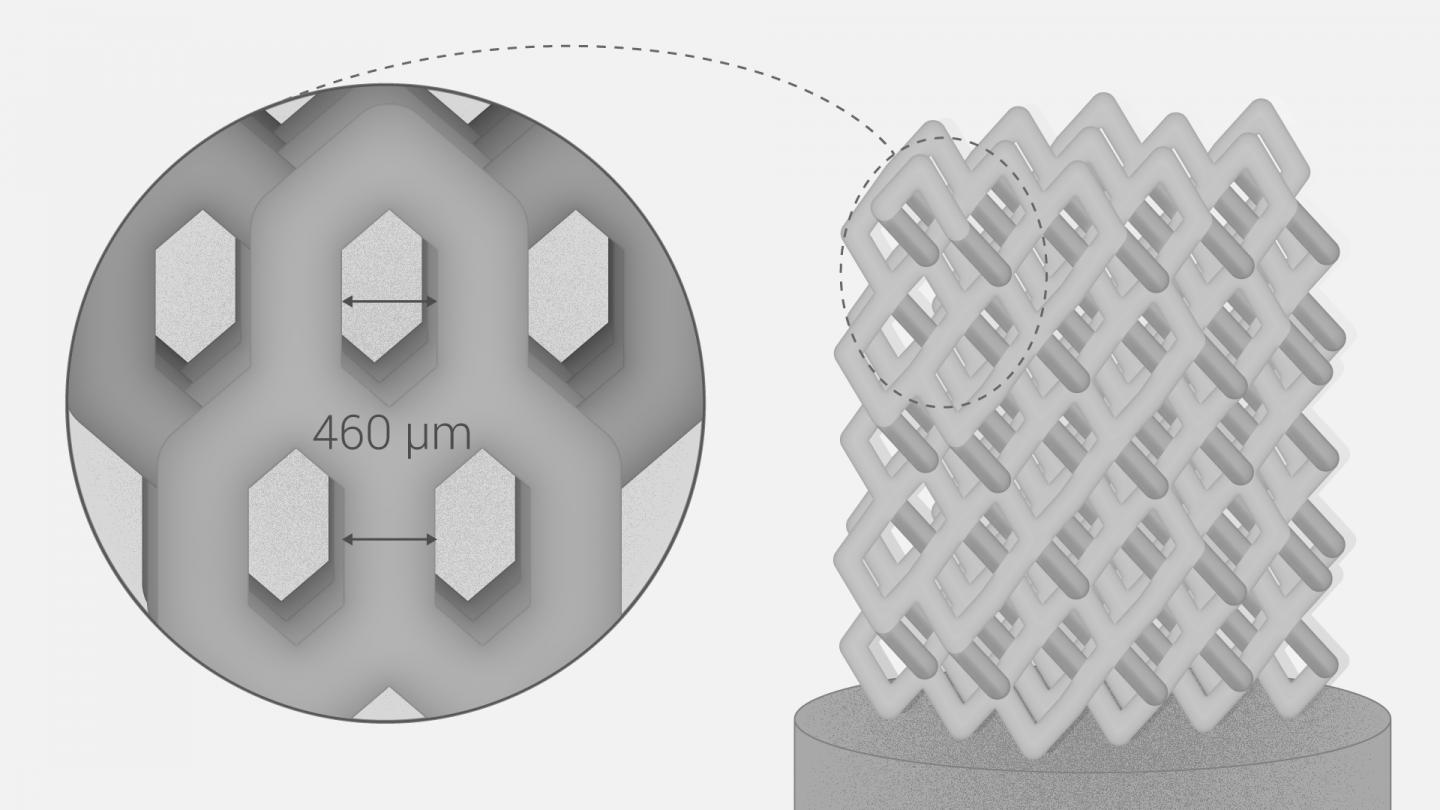
The Skoltech scientists, meanwhile, identified porosity as vital to the proliferation of cells after surgery, and narrowed the ‘optimal pore size’ down to being between 390 and 590 µm. Achieving this level of accuracy has proved difficult using existing feedstocks, as their low porosity impedes the growth of tissues, blood vessels, and other nutrient ducts.
Currently, foaming and burnt-out additives are used to overcome these limitations, but the team theorized that 3D printing would provide a better platform for creating macroporous structures. Given that additive manufacturing allows for the production of parts with controllable porosity, the technology holds the potential for printing customizable implants with a tailored structure.
The team’s FRep-optimized 3D printing method
In order to develop an implant fabrication method that allowed users to quickly personalize each and every bone graft, the scientists adopted an FRep modeling method. Essentially, FRep takes a more implicit modelling approach, which allows it to replicate complex shapes with porous, cellular, and irregular microstructures.
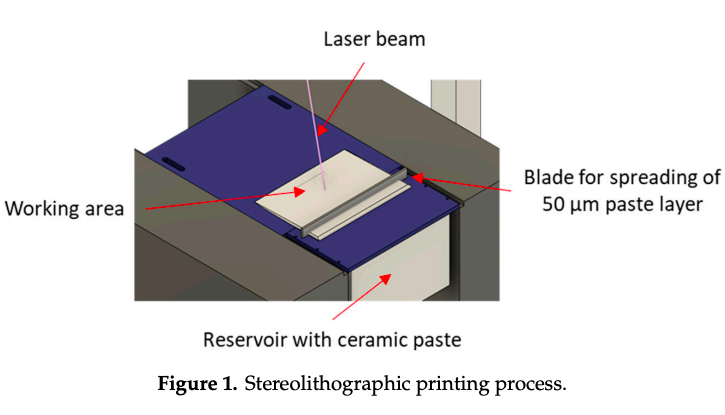
Compared to CAD-based models, the team found that FRep yielded accurate and error-free designs, that were more flexible to adaptations. To test how their models would perform in end-use conditions, the scientists used an SLA printer to cure a paste composed of a multicomponent binder and ceramic powder.
Manufacturing on Demand
Following the printing process, the ‘green’ parts were heated in a furnace to remove the plastic binder, and sintered into their final shape with predefined properties using an SLS system. The resulting cylindrical specimens were then evaluated by the team using an SEM microscopy and various mechanical stress tests.
Under axial compression, the 3D printed implants showed a strength of 400 MPa, while SEM images revealed pore sizes ranging from 440 to 700 µm (within the team’s tolerances). Although the specimens, sized 4 (D) x 9.5mm (W), proved to be self-supporting, they did require minor material reinforcement in the early design process.
Given that their implants showed the same level of compressive strength as trabecular bone, the scientists considered their approach to be a success. The team intends to optimize their printing method in future, and ten of their prototypes have been sent to an institute for animal testing with this goal in mind.
The growing additive applications of ceramics
Ceramics are increasingly being utilized to 3D print parts with enhanced properties, not just in the medical industry, but the electronics and dental sectors as well.
Material jetting specialist XJet has partnered with dentistry firm Straumann to advance the capabilities of its machines to fabricate dental products. Using both its XJet system and a ceramic-based feedstock, Straumann aims to reduce its time spent on time-intensive post-processing tasks.
The French Center for Technology Transfers in Ceramics has installed one of nScrypt’s Factory in a Tool (FiT) machines as a means of 3D printing electronics. Leveraging their new system, the team is now able to 3D print fine conductive lines conformally on various substrates.
Elsewhere, German ceramic additive manufacturing company StoneFlower3D has developed a new printhead for processing clay, concrete and pastes during 3D printing. The device is designed to provide a more accessible method of fabricating ceramic products for those with desktop machines.
The researchers’ findings are detailed in their paper titled “.” The study was co-authored by Alexander Safonov, Evgenii Maltsev, Svyatoslav Chugunov, Andrey Tikhonov, Stepan KonevOrcID, Stanislav Evlashin, Dmitry Popov, Alexander Pasko and Iskander Akhatov.
* This article is reprinted from 3D Printing Industry. If you are involved in infringement, please contact us to delete it.
Author: Paul Hanaphy

Leave A Comment