A group of researchers from Korean hospitals have carried out a retrospective study to verify the effectiveness and safety of patient-specific 3D printed titanium implants on maxillofacial bones.
A total of 16 patients were observed during the study, each undergoing reconstructive surgery for various maxillofacial defects. The patients were fitted with customized titanium implants and received long term follow-ups over the course of numerous months.
Out of the 28 implants fitted, only one failed to unite successfully with the bone while the others showed “satisfactory” outcomes for the treatment of various oral and maxillofacial defects.
3D printing maxillofacial implants
3D printing has been used to produce guides that enhance patient outcomes for some time, and has more recently began to be leveraged on an experimental basis to create facial grafts that can be implanted into patients’ skulls. For instance, scientists at Texas A&M University have developed a novel 3D printed scaffold that directly facilitates bone cell growth after surgery.
Regarding more end-use applications, the Québec Industrial Research Centre (CRIQ) has deployed a GE Additive Arcam Q10 3D printer to expedite its production of patient-specific lower jawbone implants, while researchers at Paulista University, have 3D printed a facial prosthetic for a Brazilian cancer survivor, which included her entire right eye.
More recently, Health Canada approved its first Canadian-made 3D printed medical implant, a customizable mandibular plate for use in facial reconstruction surgery predominantly for patients with oral concer.
The retrospective study
Autogenous bone grafting or implant placement is the primary method used to treat oral and maxillofacial defects, and while they are extensively biocompatible there can be issues regarding donor-site morbidity, surgical failure, and difficulty in reoperation.
Rapid advances in digital technology have opened up new avenues within the field or oral and maxillofacial surgery, with 3D printing enabling faster and accurate surgeries particularly regarding titanium materials that have already been verified for biocompatibility as dental implants.
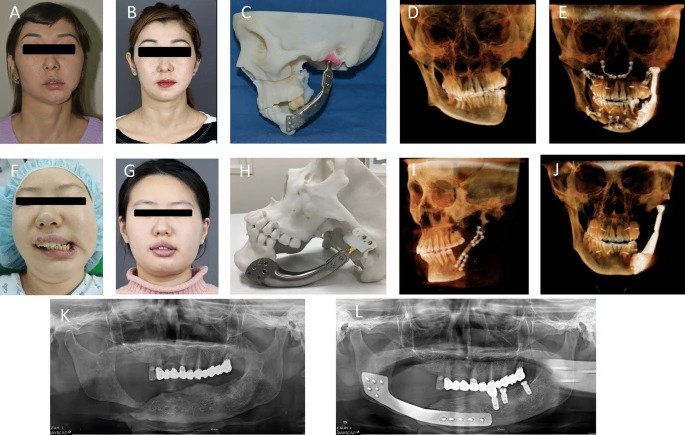
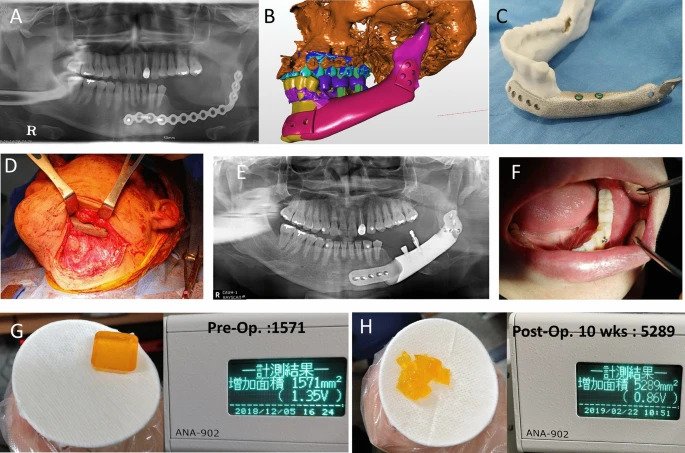
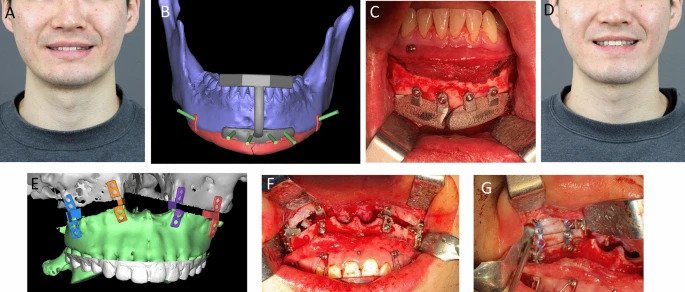
The maxillofacial titanium implants used in the surgeries that the study recorded were 3D printed via electron beam melting (EBM) and selective laser sintering (SLS) processes. 28 implants were 3D printed in total and then inserted into the maxilla (dominant portion of the face), the mandible (lower jaw) or zygoma (cheek/temple) of 16 different patients.
The patients in question, of which seven were women and nine were men, ranged in age from nine years old to 78. A total of 28 defect areas were operated on, including five mandibular segments, nine zygomas, ten mandibular bodies, angles, or chins, and four maxillary areas.
A long-term follow-up process was then conducted, varying in length per patient from eight to 79 months. The study primarily analyzed the bone fusion of the titanium implant body, but also recorded postoperative infection, implant malunion, functional results, patient satisfaction, subsidence, osteolysis around the implants, and any complications that arose.
Manufacturing on Demand
The study found that of the 28 implants, only one failed to unite with the bone. CBCT analysis showed that bone fusion at six months after surgery was 96.5 percent. The study also observed no osteolysis – a progressive condition where bone tissue is destroyed – or subsidence around the titanium implants.
According to the study, the patients that took part in the trial were on the whole aesthetically and functionally satisfied with the results of their surgery. Although, two of the five patients who had a cheekbone reconstruction underwent revision surgery due to being dissatisfied with the appearance of the implant.

Reviewing the implants
The design of the bone-to-implant interface of the 3D printed implants was either a mesh or solid based on whether stability was required. As the rough surface of the mesh titanium implant was found to be more likely to integrate into the patient’s bone, this one was preferred.
SLS enables additive manufacturing with metals such as titanium at a high sintering temperature, however, owing to limited dimensional accuracy and poor surface roughness, process improvements are being made to improve its properties. EBM uses an electron beam instead of a laser beam to sinter or to fuse the materials. EBM can be used to fabricate complex geometries by scanning each cross-sectional layer selectively, unlike SLS.
The implants 3D printed via EBM were more expensive than those 3D printed using SLS, however there was found to be no difference in the clinical results regarding the type of implant interface or the 3D printing method.
The follow-up appointments found that three out of the 16 patients experienced complications such as screw fractures and aesthetic dissatisfaction, however all of these were eventually resolved and post-operative recovery was found to be satisfactory in all patients.
Based on the patients’ experiences, the study has put forward guidelines for the use of 3D printed titanium patient-specific implants. In brief, the study advises that such implants should be used for continuity defects of the facial bone limited to hard tissue for which reconstruction has already been performed and there is no reconstruction option, and for cases where there is a mild or moderate bone defect due to previous excessive bone preparation in a patient with facial osteoplasty.
Additionally, the guidelines say that 3D printed titanium implants should also be used in cases of high aesthetic requirements such as correcting skeletal asymmetry, for areas that require functional load bearing such as the mandible, and when simultaneous reconstruction with dental implants is required.
Further information on the study can be found in the paper titled: published in the Nature journal. The study was co-authored by H. Lim, Y. Choi, W. Choi, I. Song, and U. Lee.
* This article is reprinted from 3D Printing Industry. If you are involved in infringement, please contact us to delete it.
Author: Hayley Everett

Leave A Comment