A recent collaboration between researchers at the University of Oregon (UO) and L’Oréal has resulted in the development of a multilayered artificial skin model, designed to resemble the complexity of real human skin closely.
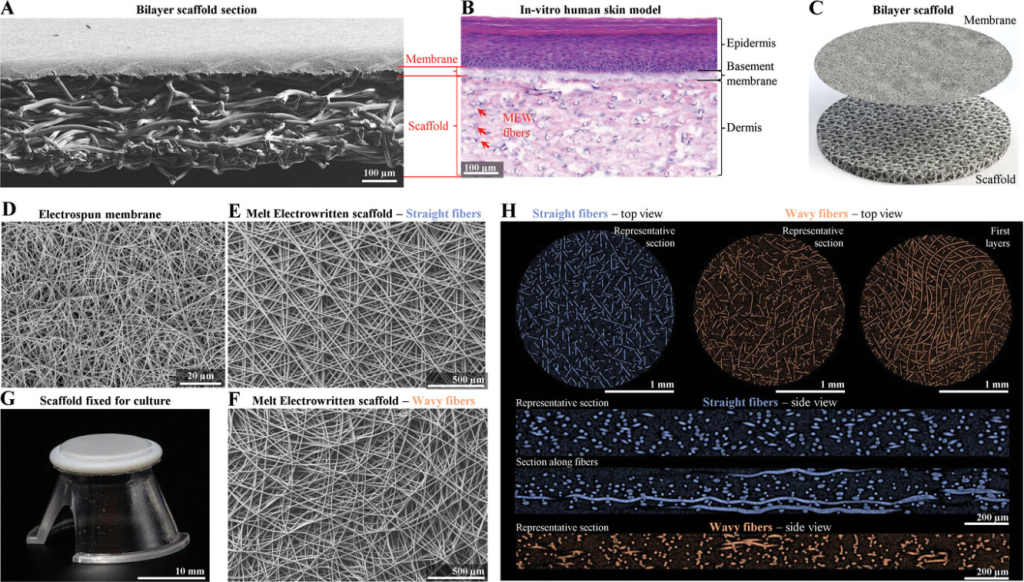
This achievement has implications for improving the testing of skin care products and potentially enhancing skin healing methods. Led by Associate Professor Paul Dalton from the Phil and Penny Knight Campus for Accelerating Scientific Impact at the UO, the research relies on Dalton’s novel 3D printing technique. Published in the journal Advanced Functional Materials, this technique enables the creation of a two-layered artificial skin, with each layer separated by a membrane, mirroring the structure of natural skin.
According to Ievgenii Liashenko, a research engineer in Dalton’s lab, this achievement is significant for its ability to reproduce different kinds of cells at full thickness while maintaining separation through the membrane.
“While we’ve made this big advance with the skin, the design of the scaffold is crucial and could be applied more broadly,” Dalton said. “There are so many diseases and injuries in the world that aren’t being solved, so having an extra tool to try to tackle these is really valuable.”
3D printing mimics skin’s anatomy
Generating artificial skin involves complexities beyond mere cell growth in a petri dish, says the team. Real skin comprises various layers housing diverse cell types, each executing specific functions. Within the body, cells rely on an external framework of proteins and molecules, known as the extracellular matrix. This intricate system aids in cell anchorage and facilitates communication among neighboring cells, essential for maintaining systemic functionality.
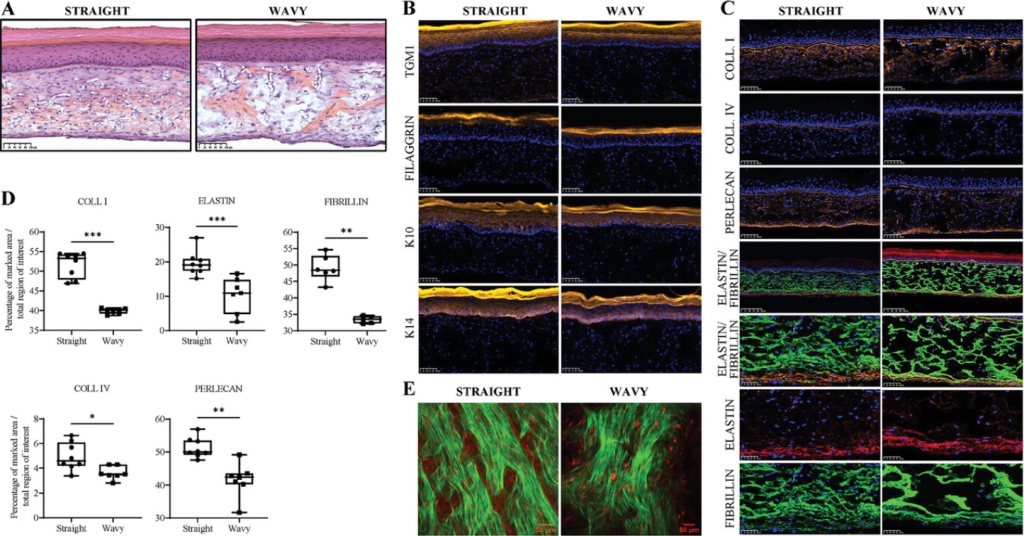
This artificial skin model is constructed using plastic scaffolds, which mimic the extracellular matrix found in real skin. Working with Dalton’s team, L’Oréal researchers grew cultured cells in these scaffolds to create artificial skin, with each layer containing different cell types. The membrane ensures that cells in each layer remain separate during development, closely imitating the natural environment of real human skin.
Developed through melt electrowriting, the scaffold of the artificial skin comprises thin threads akin to spaghetti strands, providing precise control during printing, according to Dalton. This innovative technique addresses the challenge of balancing fine detail and object size, often encountered in other 3D printing methods where resolution may diminish with larger constructs.
One of the notable advantages of this new skin model is its accelerated growth time, requiring just 18 days compared to the previous 21 to 35 days for scaffold-based artificial skin models. This efficiency makes it more feasible for commercial lab testing, a development that L’Oréal is leveraging for testing cosmetics and skincare products.
Looking ahead, both Dalton’s team and L’Oréal researchers envision a multitude of potential applications for the underlying scaffolding in skin tissue engineering. These include addressing challenges such as diabetic foot ulcers, skin grafts for burn patients, and even broader biomedical applications like artificial blood vessels and nerve regeneration structures.
Manufacturing on Demand
Importantly, the materials used in the scaffold are already FDA-approved for use inside the human body, streamlining the path to real-world application. With fabrication facilities at the Knight Campus enabling scaled-up production, Dalton emphasizes the potential for this innovation to influence research fields globally, addressing unmet medical needs with a versatile and impactful tool.
Artificial skin development over the years
In recent years, there has been growing interest and development in 3D bioprinted skin models and grafts. These breakthroughs are driven by their potential applications, including disease modeling, testing new treatments, and offering an alternative to animal testing.
Additionally, bioprinted skin has captured interest for its potential in advancing wound healing treatments. For instance, the NOVOPLASM consortium has developed cold plasma technology to treat infected burns and skin grafts, while the University of Birmingham and the University of Huddersfield developed the SLAM 3D bioprinting for treating chronic skin wounds.
Even in space, the potential of 3D printed skin is being explored. Back in 2022, astronauts aboard the International Space Station (ISS) developed bioprinted bandages from their own cells. These innovative bandages hold promise for improving the healing of flesh wounds during space missions. Elsewhere, Cornell University researchers developed a biomaterial for 3D printing artificial skin mimicking natural human tissues. Combining collagen with a ‘zwitterionic’ hydrogel, this biohybrid composite offers softness, biocompatibility, and flexibility.
You might also like:
The next generation of multi-functional ceramic surgical tools with Lithoz 3D printing technology: Designs of ceramic surgical tools have until now been strongly limited by traditional manufacturing methods, which are only economical if used for large quantities. Lithoz’s ceramic 3D printers combine a new dimension of design freedom with scalable and efficient mass production.
* This article is reprinted from 3D Printing Industry. If you are involved in infringement, please contact us to delete it.
Author: Ada Shaikhnag

Leave A Comment