In the intro to the HBO sci-fi series Westworld, a 3D printer churns out humanoid robots, delicately assembling the incredible complexities of the human form so that those robots can go on to—spoiler alert—do naughty things. It takes a lot of biomechanical coordination, after all, to murder a whole lot of flesh-and-blood people.
Speaking of: Researchers just made a scientific leap toward making 3D-printed flesh and blood a reality. Writing recently in the journal ACS Biomaterials Science & Engineering, a team described how they repurposed a low-cost 3D printer into one capable of turning an MRI scan of a human heart into a deformable full-size analog you can actually hold in your hand. Squeeze it, and it’ll give like the real thing. Slice it open, and you’ll find chambers. The idea isn’t to one day realize the homicidal humanoids of Westworld, but to give surgeons a better way to practice on a patient’s heart before an operation. The advance might eventually lead to fully-functioning 3D-printed hearts, and give medical device developers an unprecedented platform for testing their wares.
The researchers call their technique the Freeform Reversible Embedding of Suspended Hydrogels, or FRESH. They begin with a scan of a real heart and translate the data into something a 3D printer can read. Because the device works by depositing layers of material one on top of another, they run the 3D image through a slicer program. “For every layer, it basically defines the path that the material is going to be extruded, and then feeds that to the printer,” says Adam Feinberg, a biomedical engineer at Carnegie Mellon University who co-authored the new paper.

That printer churns out alginate—a squishy material derived from seaweed—that the researchers chose both for its low cost and likeness to the material properties of human heart tissue. But instead of it extruding it into air, as a normal 3D printer might do when building something out of plastic, this extrudes the ersatz heart into a container of support gel, specifically gelatin.
“The analogy I have is: Imagine you were printing inside of hair gel,” says Feinberg. Think of the little bubbles suspended in that bottle of gel—the material is providing enough support for them to float indefinitely, or at least until you squeeze the gel out of the bottle. In this case, the gelatin offers enough give for the needle of the 3D printer to slide through. “Whatever you extrude stays embedded in place, kind of like those air bubbles in hair gel,” Feinberg says.
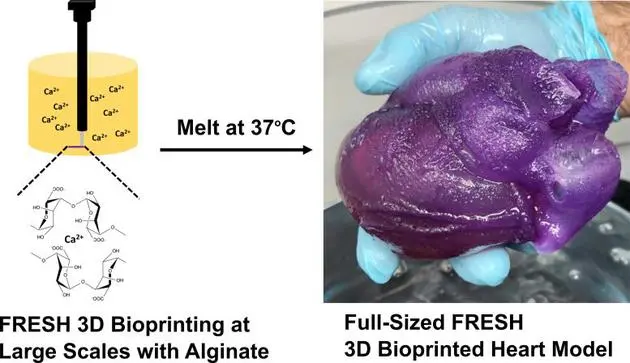
And now for something completely different when it comes to the art of artificial hearts: jello shots. After the organ is done printing, the researchers need a way to dissolve the gel lattice that’s surrounding it, and they use a familiar method. “I think a lot of people have experienced this from using gelatin in baking or making jello shots,” says Feinberg. “It’s actually a liquid when you warm it up, but it becomes a solid gel when you cool it down. And so we take advantage of that.” When they’re ready to extract the heart, all Feinberg has to do is raise the bath to body temperature, melting away the support gel and leaving behind the 3D-printed structure.
Surgeons planning operations have previously made use of 3D-printed hearts based on scans of a patients’ own organs. But those have been made the old-fashioned way: with hard plastic. This new alginate heart, by contrast, has a similar elasticity to real tissue. “When you squeeze on it or push on it, it deforms the same amount, which is obviously much more than a hard rubber or plastic,” says Feinberg. This makes it a much more realistic tool, allowing surgeons to, say, practice suturing, which would be impossible on impenetrable plastic.

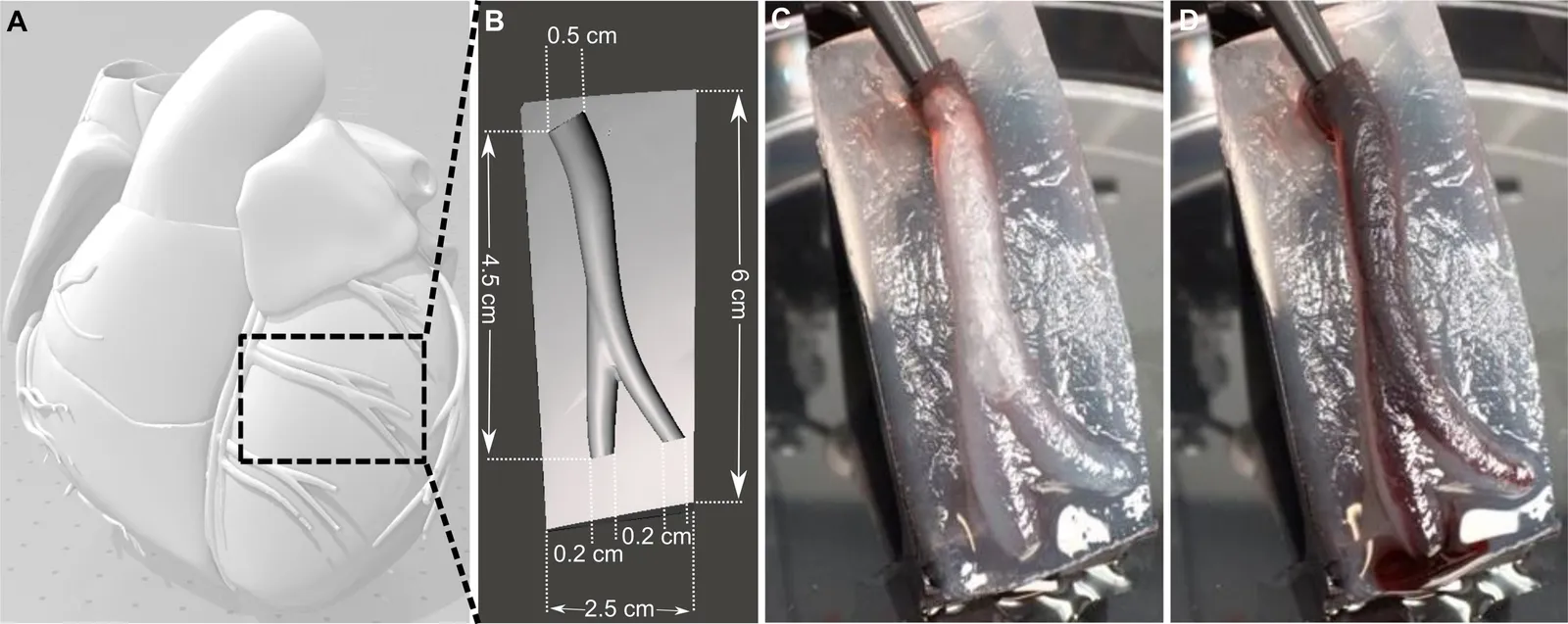
In addition, the team 3D-printed a separate section of a coronary artery using the same technique to see if it would be perfusable, or capable of carrying blood. Sure enough, when they pumped in fake blood, the artery held onto the liquid without leaking. It’s a step toward creating a heart with interconnected vasculature, Feinberg says. That way, surgeons could practice suturing arteries with blood still flowing.
In addition, this team hopes to eventually “cellularize” the printed heart, or add human heart muscle cells to the structure, to make it beat like the real thing. These are already grown in labs, where scientists take stem cells and differentiate them into heart cells. The problem, at least at the moment, is that realistically they can only make 100 million cells at a time. For a full-size heart, you’d need 100 billion cells. But, says Feinberg, “once that’s solved, we have this fabrication technology now ready to go.”
So, when might we get operational 3D bioprinted organs? “The answer is more than 10 years,” says Feinberg. “We’ve got a lot to do before we get there.” This is an intricately vascularized organ, after all, so they’ve got to scale up that work on the artery to the entire heart. And getting it to actually work as a muscle requires advances in the lab production of cells.
In the meantime, these early iterations of the printed heart could help surgeons better prepare for operations. “The fact that they’re actually having much more of a tactile fidelity is super important,” says Lillian Su, a cardiac intensive care physician who has studied 3D printing as a training tool, but wasn’t involved in this work. A surgeon could even use a custom-printed heart to communicate to a patient and their family how an operation would work. “I think that’s really the novel component, is this texture,” Su adds. “And I think that families are going to then demand to see what a surgeon’s plan will be for a given case, and that’s just going to be part of the consent process.”
In the future, hospitals could provide this on the cheap, as an alginate heart costs maybe $10 in materials. Feinberg and his colleagues also want to experiment with different materials. Printing a heart out of collagen would make it even more lifelike, since collagen already provides structure to the human body as the protein that makes up connective tissues. In fact, by dry weight, our bodies are more collagen than anything else. But the problem is that collagen is significantly more expensive—the same bioprinted heart would cost $2,000.
But in the grand scheme of a complex heart operation, $2,000 is a minimal investment. “So we’re actually thinking there are a number of applications where the more realism with the collagen is probably worth it,” says Feinberg. “But when you’re doing research in a lab—and if you’re making a lot of mistakes developing the technology—we focused on alginate for the first pass.”

Leave A Comment