Researchers have developed a groundbreaking process that enables multi-material 3D printing of realistic models of the heart’s aortic valve and surrounding structures to mimic the exact appearance of real patients.
These patient-specific organ models, including 3D printed soft sensor arrays integrated into the structure, are made using special inks and a customized 3D printing process. Such models can be used to prepare for minimally invasive surgery to improve the prognosis of thousands of patients worldwide.
Under the leadership of the University of Minnesota (UMN) and with the support of Medtronic, the research was published in Science Advances, a peer-reviewed scientific journal published by the American Association for the Advancement of Science (AAAS). Kaiyan Qiu, assistant professor at Washington State University, was a postdoctoral researcher at UMN and one of the first authors of the study.
The researchers 3D printed the so-called aortic root, which is the part of the aorta closest to and attached to the heart. The aortic root is composed of the aortic valve and the coronary artery opening. The aortic valve has three valves, called leaflets, surrounded by an annulus. The model also includes the left ventricular muscle and part of the ascending aorta.
“Our goal with these 3D-printed models is to reduce medical risks and complications by providing patient-specific tools to help doctors understand the exact anatomical structure and mechanical properties of the specific patient’s heart,” said Michael McAlpine, a University of Minnesota mechanical engineering professor and senior researcher on the study. “Physicians can test and try the valve implants before the actual procedure. The models can also help patients better understand their own anatomy and the procedure itself.”
Qiu said that this work will integrate research on additive manufacturing, materials, flexible electronics, and mechanical engineering. This is the first time that researchers have developed an aortic root model with tissue physical properties so closely that it accurately mimics its geometry and mechanical properties.
“It feels like the real thing, and it has excellent sensing functions,” he said.
The organ model is specifically designed to help doctors prepare for a procedure called Transcatheter Aortic Valve Replacement (TAVR), in which a new valve is placed in the patient’s aortic valve. This procedure is used to treat a disease called aortic stenosis, which occurs when the aortic valve of the heart narrows and prevents the valve from fully opening, thereby reducing or preventing the flow of blood from the heart into the aorta. Aortic stenosis is one of the most common cardiovascular diseases in the elderly, affecting approximately 2.7 million adults over 75 years of age in North America. TAVR surgery is less invasive than open-heart surgery to repair damaged valves.
The aortic root model is made by using the patient’s CT scan to match the exact shape. Then, using the University of Minnesota’s Visible Heart Laboratory, researchers used special silicone-based inks to 3D print it, which mechanically matched the feel of real heart tissue. Commercial printers currently on the market can print shapes in 3D, but the inks used are usually too hard to match the softness of actual heart tissue.
On the other hand, a professional 3D printer at the University of Minnesota can imitate the soft tissue components of the model and the hard calcifications on the valve flaps by printing inks similar to the spreading cream used for repairs in buildings. Drywall and plaster.
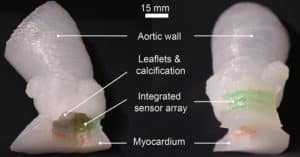
Surgeons can use these models to determine the size and position of the valve device during surgery. The 3D printed integrated sensor in the model provides the physician with electronic pressure feedback, which can be used to guide and optimize the selection and positioning of the valve within the patient’s anatomy.
Qiu said this work could lead to better surgical training for doctors, help them better predict postoperative complications, and help manufacturers improve medical equipment. He hopes to continue the research on developing 3D printed pre-operative organ models at WSU with collaborators from industry and academia. He also hopes to continue the research on 3D printing and models of biological tissues, which can one day be used to replace real tissues or organs in the body.
“This work provides limitless possibilities in the development of next-generation prostheses and medical devices,” he said.
In addition to McAlpine and Qiu, the research team also includes researcher Ghazaleh Haghiashtiani of the University of Minnesota, the first author of the study, and a recent Ph.D. in mechanical engineering. Graduate now working at Seagate; Jorge D. Zhingre Sanchez, formerly a Ph.D. in Biomedical Engineering. A student working in the Visible Heart Laboratory at the University of Minnesota is now a senior R&D engineer at Medtronic; Zachary J. Fuenning, a graduate student in mechanical engineering; Paul A. Iaizzo, a professor of surgery at the School of Medicine, and the founding director of the University of Visible Heart Laboratory; Priya Nair, senior scientist at Medtronic; and Sarah E. Ahlberg, director of research and technology at Medtronic.
This research was funded by Medtronic, the National Institute of Biomedical Imaging and Bioengineering of the National Institutes of Health, and the Minnesota Discovery, Research and Innovation Economy (MnDRIVE) program in Minnesota. The University of Minnesota Interdisciplinary Doctoral Scholarship and Doctoral Dissertation Scholarship were provided to Ghazaleh Haghiashtiani.


