The Veterans Affairs (VA) Puget Sound Health Care System, a network of medical centers under the Veterans Health Administration (VHA), and the University of Washington School (UW) of Medicine recently announced a two-year partnership aiming to advance medical 3D printing. Both organizations are collaborating to develop new applications for 3D printing in the diagnosis and treatment of complex heart conditions.
As part of the agreement, both organizations will share 3D printers, 3D materials, software and staff (physicians, researchers and engineers), with the goal of quickly developing new protocols for operational planning procedures using the technology. Examples include creating patient-specific 3D printed models to help treat mitral valve disease, a complex heart abnormality. Dr. Beth Ripley is a VA Puget Sound radiologist, VHA Senior Innovations Fellow and VHA 3D Printing Advisory Committee chair. Speaking to 3D Printing Industry about the recent partnership, Dr. Ripley explains her view for the future of 3D printing in hospitals and medical care.
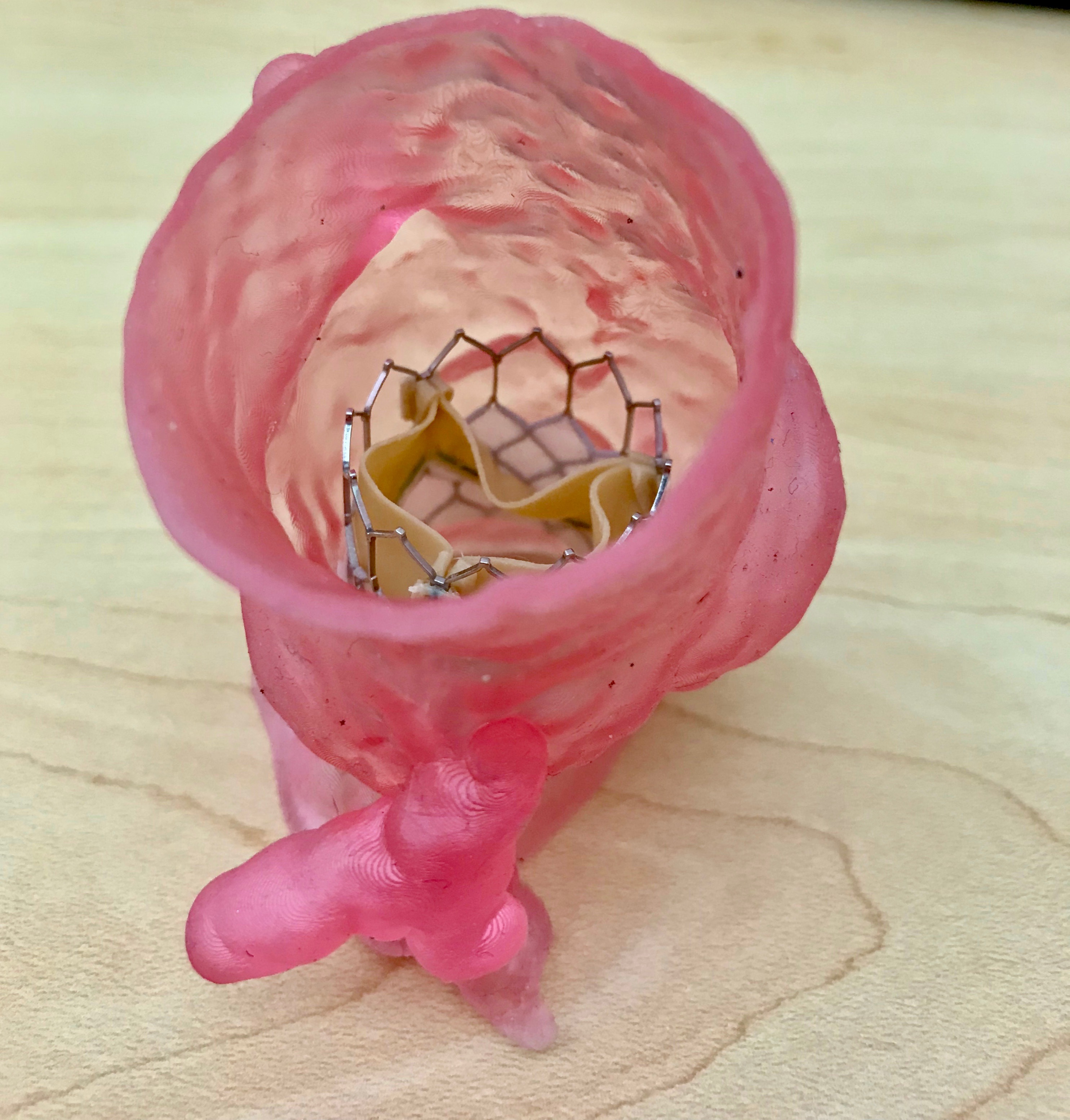
“Imagine the power of holding a life-sized 3D model of your own heart in your hands while your cardiologist discusses your treatment plan and walks you through your upcoming procedure step by step. This is the reality that we want for all of our patients,” comments Dr. Ripley.
“As the largest integrated healthcare system in the United States and one of the largest hospital-based 3D printing networks, the VA is defining how 3D printing is being used now and how it will be used in the future.”
The VA Puget Network and VHA 3D Printing Network
The VA Puget network covers VHA medical centers serving the Seattle and Tacoma areas of Washington state, providing healthcare to over 105,000 veterans living in 14 counties around the Puget Sound in the Pacific Northwest. Focusing on innovation in providing healthcare to veterans, VA Puget Sound has demonstrated a continuous effort in bringing 3D printing to patient care.
Serving as the flagship site of VHA’s 3D Printing Network, which began in 2017, it has led workshops on 3D printing in medicine, and undertaken collaborations with the likes GE Healthcare to improve clinical outcomes and medical treatment for veterans using 3D printing. The hospital’s 3D printing network has grown to contain 20 hospitals in the past two years. The benefits some of these hospitals have already gained include the production of model kidneys to inform pre-surgical planning, and specialized foot orthotics that help prevent avoidable amputations.

3D printing patient-specific models for any complex anatomy
The UW School of Medicine is home to a nationally recognized 3D printing lab that has produced over 100 patient-specific models for cardiologists and surgeons. Research Scientist Dmitry Levin, who manages the lab, says that by partnering with VA Puget Sound, “we merge all of our collective expertise into a unified effort to offer patients personalized cardiac care based on their unique needs.”
Together, UW Medicine and Puget Sound seek to improve access to invasive treatments like transcatheter aortic valve replacements (TAVRs). Surgical outcomes are also expected to improve under the partnership, as 3D printing enable cardiologists to better visualize each patient’s unique anatomy. “Patient-specific 3D models are created from cross-sectional imaging studies, most commonly CT or MRI scans,” explains Ripley. “We verify the accuracy of the models by confirming that the 3D model dimensions match the imaging dimensions. This is part of our quality assurance practice, which underpins all that we do to ensure the best health outcomes for our patients.”
Manufacturing on Demand
Initially, the partnership will focus on using 3D printing to create cardiac models, however, it will also expand to comprise any part of the body. Dr. Ripley comments that “VA Puget Sound and UW Medicine will print patient-specific models for any complex anatomy, from head to toe. This includes the brain, skeleton and heart, as well as abdominal and pelvic organs.” She adds that the team will first focus “creating standardized pathways” for heart models as these are in the highest demand. In addition, Dr. Ripley states, “Patient-specific 3D models are being printed in the medical centers at VA Puget Sound and University of Washington. The majority of models will be printed at the facility where the patient is receiving care.”
Both UW Medicine and VA Puget will use the FDA-cleared Mimics 3D printing software from Materialise to create their medical models, as well as GE Advanced Workstation Volume Share software. VA Puget Sound will be providing its selection of 3D printers, including the F370, Mojo, Objet 30 and Objet 350 Connex3 3D printers from Stratasys, and the Formlabs Form2. UW Medicine on the other hand also has the Formlabs Form2, as well as 3D printers from Dremel, NewPro 3D, Uniz, Prusa and Z Corporation (now 3D Systems).
Helping hospitals adopt 3D printing on a global scale
The developments and results of VA Puget and UW Medicine’s research agreement are expected to create benefits that extend beyond VA’s 9 million enrolled patients and UW Medicine’s broad geographic patient base. Both organizations hope to inform future research, and help to develop and scale 3D printing applications for advanced treatments on a global scale. When asked how the two organizations plan to help hospitals outside their own networks adopt 3D printed models, Dr. Ripley states that establishing best practices is key, “Once we have created and validated standardized workflows for creating 3D models, we plan to share them with the community through publications, hands-on courses offered at academic meetings and free online content,”
“The goal is to encourage best practices in 3D printing as this field grows.”
“In the near future,” Dr. Ripley adds, “we anticipate significant growth in the number of both public and private hospitals acquiring 3D printers. And we hope the workflows we create will help facilitate adoption of best practices at these new health care facilities.”
Dr. Ripley believes that the next big step for 3D printing in medicine now lies with bioprinting and developing it for FDA-clearance. Despite being a long way off, the ultimate goal for VA is to create tissues and organs that can integrate into a patient’s body. However, the short-term goal for bioprinting revolves around creating living, vascularized bone.
“The hope is that, in the future, we could create replacement organs that could address the unmet need for transplant organs,” Dr. Ripley concludes, “Our short-term goal is to be able to 3D print living bone that can grow and merge with the patient’s bone. This could be used to replace bone that is lost from infection or malignancy. For this to become a viable technology, we need to perfect the process of printing bone and demonstrate to the FDA that it is safe and effective.”
* This article is reprinted from 3D Printing Industry. If you are involved in infringement, please contact us to delete it.
Author: Anas Essop

Leave A Comment