A team of researchers from Duke University and Penn State, led by Julia Oh, PhD, and Ibrahim Ozbolat, PhD, is using a 3D bioprinted lung model to study how influenza and bacteria interact in human lung tissue. Funded by a $3.2 million NIH grant over four years, the project aims to uncover why some co-infections worsen illness, with experiments conducted in labs at Duke and Penn State.
“Researchers have long studied the flu virus’s effects on the lungs, but we don’t know how adding diverse bacterial strains changes the outcome,” said Oh. “The respiratory microbiome varies widely between people, and we’ve lacked models that reflect that complexity.”
3D Bioprinting Offers Real-Time Insights into Respiratory Infections
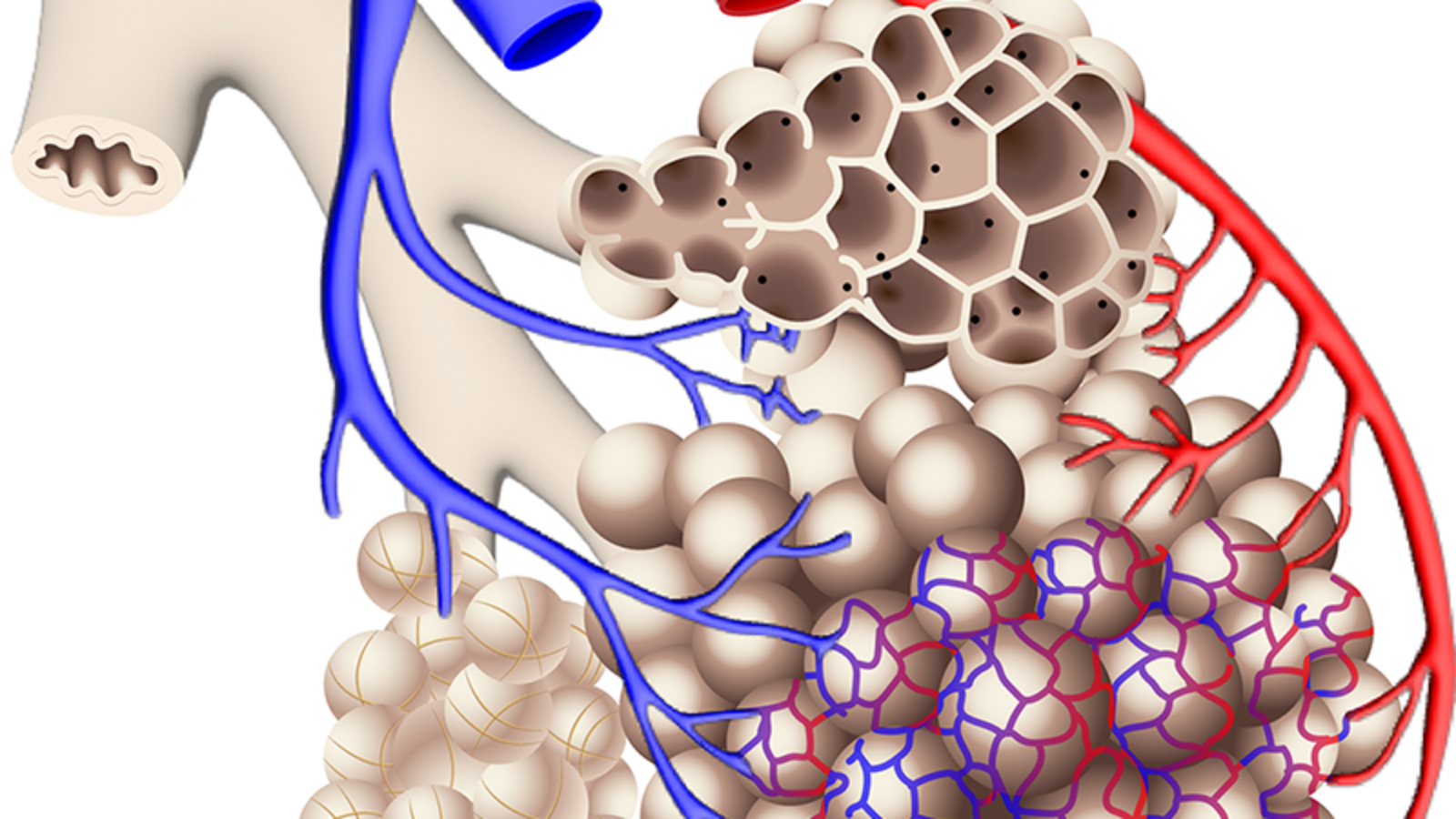
The study uses a 3D bioprinted lung system developed in Ozbolat’s lab. Constructed from stem cell–derived lung cells, the miniature tissues can be ventilated like real lungs, allowing viruses and microbes to be introduced while infections are observed in real time.
“The precision of bioprinting lets us recreate miniature, breathing lung sacs that behave like native tissue,” Ozbolat said. “This is the first time a dynamic 3D lung model will be used to study virus–bacteria interactions.”

Ozbolat’s team will generate the bioprinted tissues at Penn State, while Oh’s team at Duke will infect them with influenza and selected bacterial strains. Using multiomics analysis and advanced imaging, the researchers hope to identify why some co-infections worsen illness and why others may stimulate immune defenses.
Given influenza’s widespread impact, the findings could inform future vaccines and therapies. The model also offers a new way to study respiratory infections without relying on animal or human testing. The project includes collaborators from the Jackson Laboratory and Nationwide Children’s Hospital.
Manufacturing on Demand
3D Bioprinted Lungs Simulate Extreme Environments
Researchers at Texas A&M University are using 3D bioprinting to study how human lung cells respond to extreme pressure, temperature, and oxygen changes encountered at high altitudes and in space. Led by Dr. Zhijian “ZJ” Pei and Dr. Hongmin Qin, and funded by the U.S. Air Force Office of Scientific Research, the project aims to improve aviation and spaceflight safety while advancing respiratory disease research. “By investigating how 3D bioprinted samples embedded with lung cells respond to physical stress, we’re advancing the fundamental principles of the effects of extreme environments on human biological systems,” Pei said.

Elsewhere, Canada-based Tessella Biosciences, a McMaster University spinout, has created a novel bioink that enables 3D printing of soft lung tissue capable of expanding and contracting like real lungs. The material remains stable at body temperature, producing flexible, stretchable structures in under an hour, making it a more accurate in vitro model for respiratory disease research and therapeutic testing.
You might also like:
Maxwell Clinic Integrates Advanced Dentistry to Support Airmen Readiness: The core mission of the dental flight remains maintaining the readiness of active-duty members.“The unit’s overall mission is to make sure that our active-duty members are able to be fit and ready,” said U.S. Air Force Tech. Sgt. Ernessie Ladouceur, Maxwell Medical Group dental flight chief. “So that way when they’re out there, they’re not having to worry about something like a toothache.”
* This article is reprinted from 3D Printing Industry. If you are involved in infringement, please contact us to delete it.
Author: Paloma Duran

Leave A Comment