U.S. private research university Carnegie Mellon University has received up to $28.5 million from the Advanced Research Projects Agency for Health (ARPA-H) to develop a 3D bioprinted, immune-compatible liver designed to temporarily support patients with acute liver failure, potentially reducing the need for full organ transplants and advancing regenerative medicine.
“The goal is to create a piece of liver tissue that you can use as an alternative to transplant, specifically for acute liver failure,” said Adam Feinberg, professor of biomedical engineering at Carnegie Mellon and principal investigator. “The liver we are creating would last for about two to four weeks. It would give patients time for their own liver to regenerate, and then, they would not need a liver transplant, freeing up those livers for other patients. The liver is just the first application, with the plan to expand to the heart, pancreas, and other organs. This innovation would fundamentally change healthcare as we know it, because most people suffer at some point from end-stage organ failure.”

Collaboration and Advanced Bioprinting
The project, called Liver Immunocompetent Volumetric Engineering (LIVE), is co-led by Kelly Stevens, professor of bioengineering at the University of Washington, and involves experts from Charité – Universitätsmedizin Berlin, FluidForm Bio, Iowa State University, Mayo Clinic, the University of Pittsburgh, and Carnegie Mellon University.
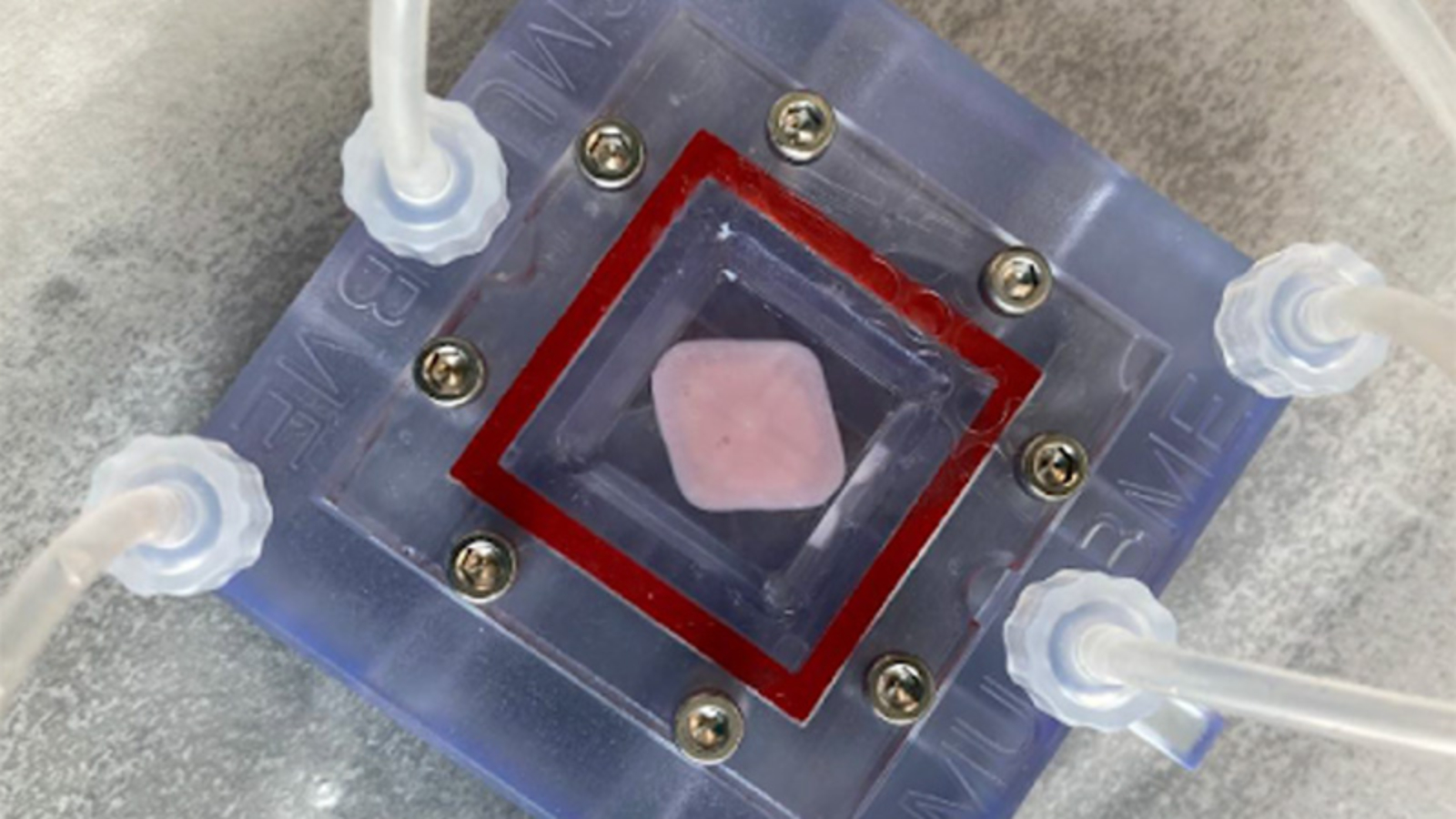
The team will use Carnegie Mellon’s FRESH 3D bioprinting and 3D ice printing platforms to construct livers entirely from human cells and structural proteins like collagen. The organs are designed to be immune-compatible, reducing or eliminating the need for immunosuppressive drugs. “The challenge is really the immune system,” Feinberg elaborated. “We are going to be using hypoimmune cells, which are engineered to be a universal donor, so anyone can have the cells and tissues we are building without needing to take immune suppression.”
Within five years, the team aims to produce adult-scale livers ready for pre-clinical testing and eventual human trials. “The LIVE project is going to significantly advance organ biofabrication for transplant by funding our highly capable team that combines the very best engineers, biologists, and clinicians,” Feinberg added. “The technologies and capabilities we develop will also have an impact beyond the liver, enabling additional efforts to build human tissue and organs to treat congenital heart defects, heart disease, blindness, and Type I diabetes.”
Manufacturing on Demand
Advancing Regenerative Medicine Through 3D Bioprinting
Building on similar regenerative goals, UT Southwestern Medical Center (UTSW) is leading a federally funded initiative to produce functional liver tissue using 3D printing. Supported by ARPA-H with up to $25 million over five years, the Vascularized Immunocompetent Tissue as an Alternative Liver (VITAL) project also falls under the Personalized Regenerative Immunocompetent Nanotechnology Tissue (PRINT) program. The effort aims to address organ shortages, reduce high transplantation costs, and minimize the need for long-term immunosuppression. Researchers collect patient-derived cells, convert them into induced pluripotent stem cells, guide them to differentiate into liver cell types, and combine them with hydrogel bioinks to bioprint functional tissue for transplantation, pharmaceutical testing, and research.

Elsewhere, U.S.-based 3D printer manufacturer 3D Systems, in collaboration with French MedTech firm TISSIUM, received FDA approval for COAPTIUM CONNECT with TISSIUM Light, a bioabsorbable, 3D printed device designed to repair peripheral nerve damage and promote tissue regeneration. The sutureless, atraumatic implant leverages TISSIUM’s biomorphic polymers and 3D Systems’ advanced bioprinting technology to create high-resolution, biodegradable structures that support nerve healing. Like the liver initiatives, this development underscores the transformative potential of AM in creating functional, patient-specific tissues for regenerative medicine across multiple organ systems.
You might also like:
New 3D Printed Device Helps Gaza Doctors Treat Severe Injuries: Used to stabilize complex bone injuries, the device is normally imported, typically costs more than $500, and depends on established supply chains and reliable power. In Gaza, where more than 90% of health facilities have been damaged or destroyed and hospitals operate with severely constrained electricity and logistics, such equipment has become difficult or impossible to obtain.
* This article is reprinted from 3D Printing Industry. If you are involved in infringement, please contact us to delete it.
Author: Paloma Duran

Leave A Comment