3D printed surgical guides and virtual surgical planning (VSP) have been used in many types of surgery, such as knee replacement, spinal surgery, and reconstruction of the chest wall and face. However, when it comes to the reconstruction of complex maxillofacial deformities, this kind of computer-assisted technique is usually used for bone reconstruction more often than for soft tissues. A group of researchers from the University of Michigan published a paper, “Using a 3D Printed “Phantom of the Opera” Soft Tissue Surgical Guide for Complex Facial Reconstruction,” introducing their use of VSP and 3D printed guidelines to help a injured patient suffering complex soft tissue damage from a gunshot wound.
“In ballistic injuries, there is often disfiguring damage to the soft tissue, with the destruction of anatomic landmarks making satisfactory soft tissue reconstruction a unique challenge,” the abstract states. “By combining tangible surgical models and aesthetic judgment in a team setting, it is possible to optimize the efficiency and accuracy of soft-tissue reconstruction in the setting of complex facial deformities.”
Reconstruction of ballistic facial injuries is extremely challenging, because bone tissue and soft tissue have been destroyed, and there are often tissue burns and contamination. In their study, the researchers introduced a case that integrates VSP, 3D printed surgical guides, and anaplastology—a branch of medicine dealing with the prosthetic rehabilitation of an absent, disfigured, or malformed anatomically critical location of the face or body—to provide a 19-year-old female patient with “improved facial symmetry and orbital prosthesis accommodation.”
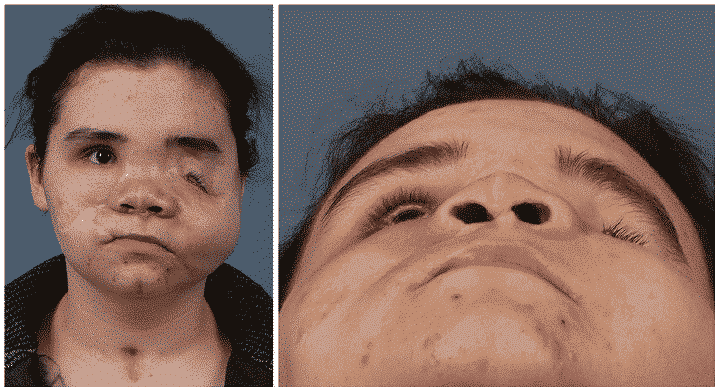
Initially, the patient went to another hospital and showed severe facial injuries such as a ruptured left eyeball and bilateral orbital fractures, bones, maxilla, nasal bone, and diaphragm. There, she underwent a tracheotomy and “multiple facial washes”, the fracture was fixed, and her left eye was removed. Unfortunately, she later suffered from a painful “bilateral macular anterior skin fistula” and was transferred to U Mich Hospital for further reconstructive surgery.
The team uses “free tissue transfer” to reconstruct all facial wounds of the patient, which will close the fistula and help rebuild its soft tissues. Although this helped relieve her pain, it, unfortunately, made the left side of her face heavier, which when used in conjunction with gravity can cause severe asymmetry. Therefore, they moved from wound control to “restoring her facial contours” and obtained her orbital prosthesis.
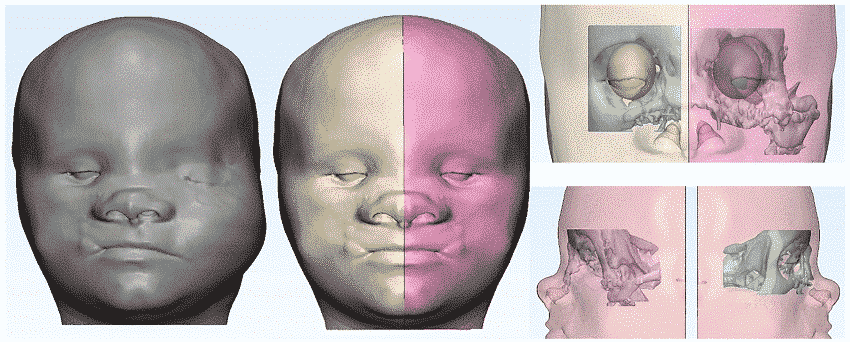
They combined the VSP mirroring technology with the proposed prosthesis size and 3D printed custom surgical guidelines to promote “precise reduction and resuspension of left macular soft tissue and periorbital soft tissue.” The researchers used Materialize Mimics to separate the relevant bone and soft tissue anatomy, and then imported the image into 3Matic to create a clear model. Use qualitative and quantitative measurements to find a “symmetrical sagittal plane” on which the unaffected part of the patient’s face is mirrored to the left.
They wrote: “The resulting shape of the left eyeball was edited to the specific size of the prototype eyeball prosthesis provided by our plastic surgeons.”
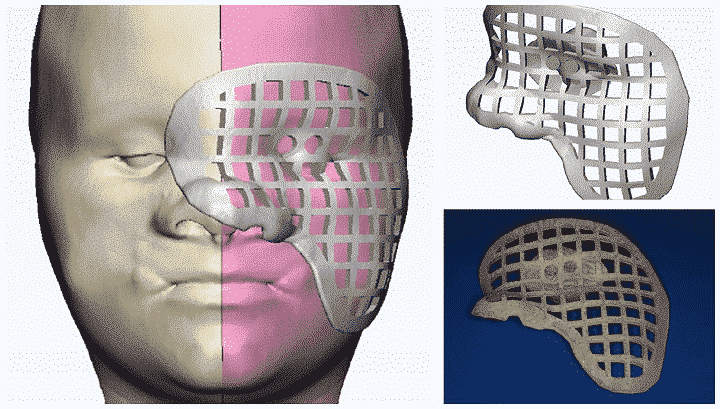
The patient approved the virtual image for the reconstruction of his plan, and made a 3D custom guide for the “reduced left orbit of the operation” and another guide for the “left eye macular reconstruction and suspension surgery”. If you are familiar with the “Phantom of the Opera” musical, the second 3D printed surgical guide will be similar to the mask worn by the Phantom herself.
In order to maximize the use of the guide during the operation, 2 posts were added to the outer surface of the rail guide, and 2 matching slots were created on the inner surface of the macular mask. The researchers explained that this allows separate or combined implantation of guide plates according to intraoperative needs. “A square cell was also cut from the malaria mask to form a grid. When the guide is installed in place, the grid will allow the surgeon to visualize the patient’s face. ”
The guide is printed on Form 2 with biocompatible Dental SG resin. I will omit all the details of the surgery, but it is enough to show that the operation has been successful. Eight months later, the patient showed that “her midface and periorbital area are symmetrical.”
They wrote: “Although we only conducted a limited follow-up of one patient, this case demonstrated the new application of computer-assisted technology and increased the equipment of maxillofacial surgeons.”
Although the matter has been resolved, there are still challenges in using computer-assisted technology to reconstruct soft tissues, such as the “natural irregularities” of the face and the fact that soft tissues are very sensitive to inflammation and dynamic changes, which means that they cannot be completely fixed.
The researchers explained: “In this way, the deformation force and the involuntary activation of facial muscles during the imaging process will distort the measurement results and cause inaccurate calculations.”
“Therefore, surgeons must still use their own judgment and consider the long-term effects of scar tissue and gravity when developing virtual models.”
In addition, if the hospital has not yet adopted VSP, 3D printing and CAD/CAM technology, it may increase costs. But in general, I call this a success story.
The research team concluded: “Although it cannot replace clinical judgment, computer-assisted technology can produce better and more accurate results, and soft tissue reconstruction should be considered.”

