Researchers at North Carolina State University have utilized 3D printing to develop more comfortable radiation-receiving antennas for cancer patients to wear during microwave breast hyperthermia procedures.
Compared to mainstream radiotherapy gear, the team’s flexible new receiver is less bulky and can be printed into patient-specific geometries, allowing it to reduce discomfort in the course of treatment. By tweaking their antenna’s level of infill, the scientists also found they were able to adjust its dielectric constant, optimizing its performance for different levels of exposure via an electromagnetic (EM) simulator.

Making radiotherapy more palatable
Microwave breast hyperthermia is a type of cancer treatment, in which affected tissues are exposed locally to a highly focused EM radiation beam that impairs malignant cells by thermal ablation. While the procedure is non-invasive, it currently requires the use of heavy antennas, which make an already-unpalatable treatment even less comfortable for patients.
In the past, significant research has been conducted into wearable alternatives, but these have largely been confined to manually-produced textiles or unwieldy water-cooled devices. Over the last few years, however, scientists have increasingly adopted 3D printing to more rapidly produce antennas, which boast enhanced flexibility and therefore patient comfort than many conventional designs.
Similarly, in their own previous research, the North Carolina team have found that they can improve the antenna gain of cotton devices by raising their porosity. Now going one step further, the researchers hypothesize that it could be possible to manipulate the infill of receivers even more, so that they’re not just comfortable, but feature optimized heating performance and cancer-fighting efficacy.
Fabricating radiation receivers
Given that adjusting the dielectric properties of antennas is critical to optimizing their performance, the scientists set about establishing exactly how they’re affected by their level of infill. To accomplish this, the team used a Luzbot Taz 6 FDM 3D printer to produce three different TPU-based devices, which featured varying volume percentages of 40%, 70% and 100%.
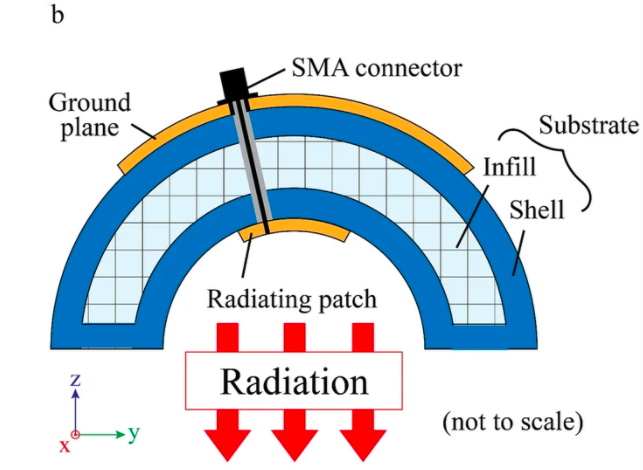
Composed of a conductive patch mounted onto a dielectric substrate, the researchers’ antennas featured a 3 mm-thick TPU top-layer, to prevent them from making direct contact with a patient’s skin. During usage, the devices’ patches are theoretically capable of relaying microwave radiation towards the center of naturally-hemispheric breast tissues, heating cancerous cells up to 39–45 °C and rendering them inert.
To test the efficacy of their novel radiotherapy devices, the North Carolina scientists attached them to a lab-made 50mm-radius ‘breast phantom,’ and subjected them to extensive EM simulations. Interestingly, the team found that reducing their antenna’s infill percentage from 100% to 43.6% lowered its dielectric constant from 2.36 to 1.59, and that this relationship was predictable as well as linear.
Manufacturing on Demand
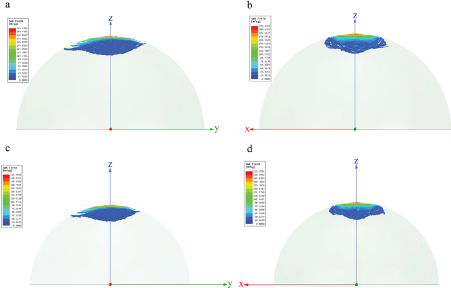
Additionally, both the 70% and 100% volume devices exhibited a resonance of 2.30 GHz and delivered a radiation absorption rate of 35-60 W/kg in 5-7mm deep tissues, well within the 8-83 W/kg recommended for hypothermia applications. However, each of the antennas also proved ineffective on tissues deeper than 15mm, and the 40%-infill prototype wasn’t sufficiently stable to maintain its hemispheric shape.
As a result, the researchers concluded that they had successfully calculated the linearity between the dielectric constant and solid volume percentage of their radiotherapy receivers, but they weren’t deployed within in-vitro applications, and if they were to be, they’d be limited to treating superficial areas of the breast.
“The employed breast phantom was homogeneous and did not precisely mimic the actual biophysical representation of the human body,” said the scientists in their paper. “There are innumerable components in real female breasts, all of which could influence heating efficacy. For a further study, it is thus indispensable to consider a more realistic phantom.”
3D printed breast cancer remedies
Whether it be 3D printed polymeric guides that enable increased tissue retention, or patient-specific bioprinted implants, researchers continue to find new ways of aiding the recovery of breast cancer survivors. Clinicians at the Korean Asan Medical Center, for instance, have combined scanning with 3D printing to create customizable surgical guides, which improve outcomes for mastectomy patients.
Elsewhere, Israeli 3D bioprinting firm CollPlant has been prototyping breast tissue-regenerating implants since at least 2019. The company believes that in future, its collagen-based grafts could provide patients with a safer alternative to more conventional methods of permanent breast implantation.
Similarly, 3D printed scaffold developer BellaSeno has agreed a deal with Evonik, to use its RESOMER polymer as a basis for a line of ISO-certified Senella breast implants. Ultimately, the firm aims to improve procedures for breast reconstruction, augmentation and revision surgery, by creating implants that can safely be absorbed by the body.
The researchers’ findings are detailed in their paper titled “,” which was co-authored by Yusuke Mukai, Sixian Li and Minyoung Suh.
* This article is reprinted from 3D Printing Industry. If you are involved in infringement, please contact us to delete it.
Author: Paul Hanaphy


Leave A Comment