Clinicians at the Dana-Farber Cancer Institute, Brigham and Women’s Hospital, Massachusetts General Hospital, and MIT have developed a novel 3D printed shielding that protects the healthy tissues of cancer patients during radiotherapy.
Using patient CT scans and high atomic number materials, the team has been able to 3D print customized devices that prevent gamma and X-ray-induced radiation toxicity in gastrointestinal or oral tissues. If used to treat head, neck, or prostate cancer patients, the scientists believe that their shielding could help reduce radiation of the mouth and stomach by up to 30% and 15% respectively, without lowering the dosage to the tumor.
“When we treat patients with radiation it’s a fine balance. We want to administer the most dose we can to shrink the tumor without causing damage to healthy tissue,” said James Byrne, a Senior Resident Physician in Radiation Oncology at Brigham, MGH, and the Dana-Farber Cancer Institute. “Our goal through this project was to find an innovative solution that could offer personalized protection for patients.”
“This personalized approach could be applicable to a variety of cancers and holds the potential to reduce the burden of radiation injury and toxicity for our patients.”
Treating radiation toxicity
Statistically, more than half of all cancer patients will undergo some form of radiation therapy, but while the treatment is effective at killing tumor cells, it can also cause toxicity to otherwise healthy tissues. In the U.S. alone, more than 200,000 patients suffer from radiation-induced oral mucositis, esophagitis, and proctitis each year, sometimes in severe enough bouts to cause them to discontinue their treatment altogether.
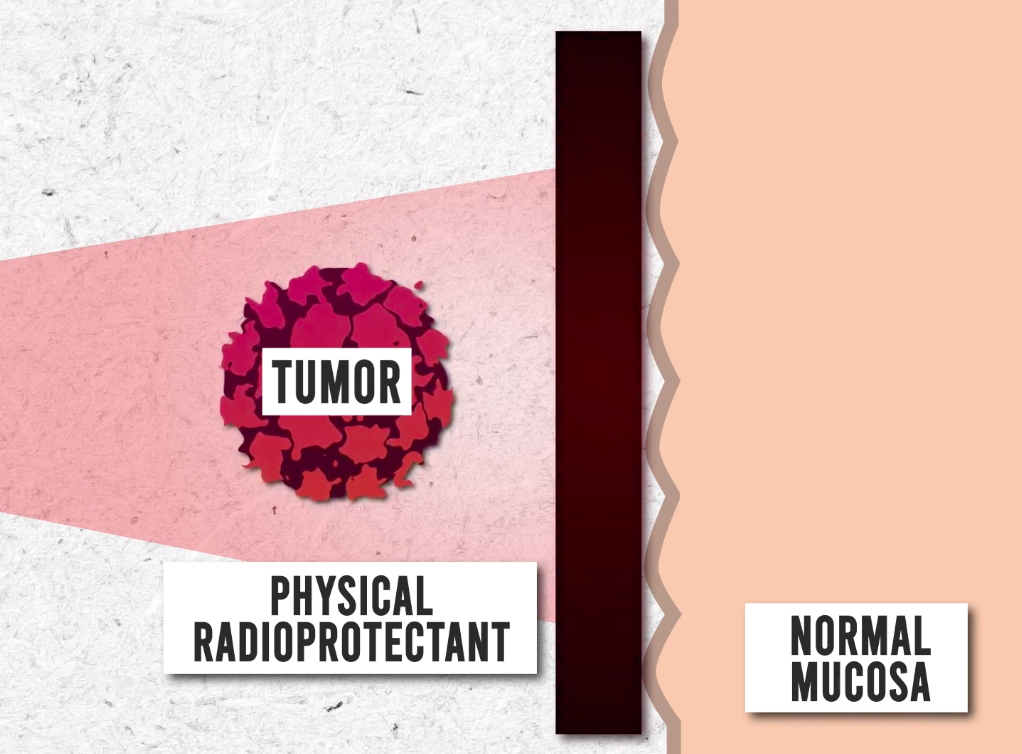
Currently, doctors tend to use physical spacers in an attempt to prevent mucositis, but these often offer limited protection, and can even lead to additional side effects. In order to reduce radiation therapy’s morbidity without limiting its efficacy, the team has therefore identified the need for patient-specific shielding that makes treatment more palatable, thus improving patient adherence and ultimately their chances of survival.
“It’s not uncommon for gastroenterologists to be called in to consult on a case to support a patient who is experiencing side effects of radiation in the esophagus, small intestine, or anywhere else in the gastrointestinal tract,” said study co-author Giovanni Traverso. “A couple of years ago, James and I began brainstorming — what if we could develop a shield that could help protect a significant portion of normal tissue in the radiation field?”
Radioprotectant 3D printing
Given that radiation‐induced toxicity is often highest in oral, lung, and prostate cancer patients, the clinical researchers opted to develop shielding that’s specifically designed to protect tissues in those areas. However, before they could set about 3D printing their radioprotective devices, the scientists needed to identify the optimal ‘high-Z material base for the task.
Initial testing, which involved exposing various alloys and plastics to 6 MV photon radiation, revealed that elemental materials provided the highest attenuation, leading the team to develop a lead and bismuth-loaded resin. Once they’d formulated their feedstock, the scientists utilized diagnostic ‘DICOM’ CT scans to create accurate 3D models of the mouths, intestines, and rectums of multiple different lab rats.
Interestingly, the resulting models revealed drastic differences in the test patients’ anatomies and allowed the scientists to personalize each device, enabling their comfortable insertion, as well as optimizing their radiation protection. The shielding itself was then fabricated using a Formlabs Form 2 3D printer, and inserted orally into seven specimens, with the aim of protecting 50% of the tissue that’s normally at risk of radiotoxicity.
Manufacturing on Demand
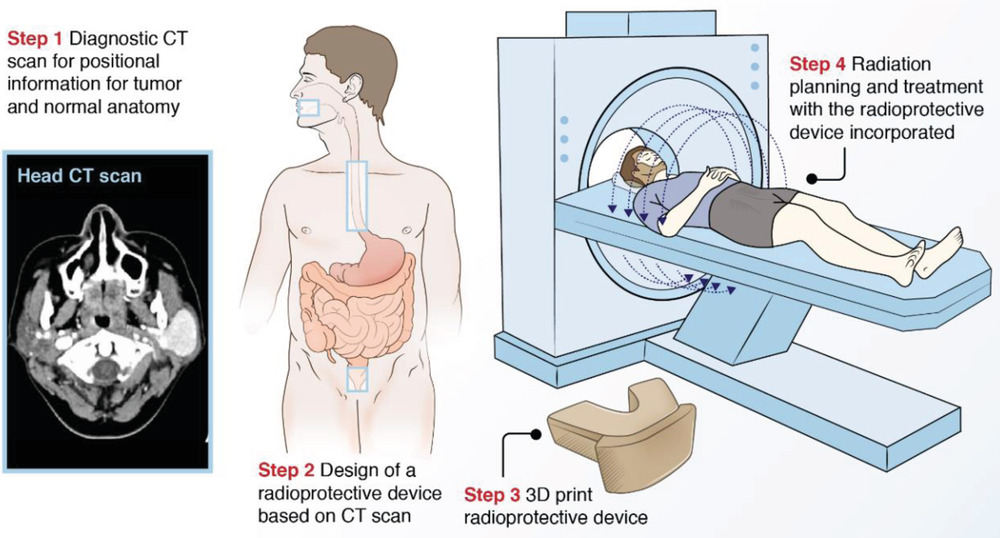
While seven unshielded rats developed radiation-induced tongue ulcers, the seven protected test subjects suffered no side effects at all. During later experiments, a similar set of intra‐oral, esophageal and rectal devices were inserted into swine specimens, which served to reduce intestinal radiation by up to 15%, and toxicity within the oral buccal mucosa by 30%, without impacting on tumor dosage.
Compared to conventional hydrogel spacers, the clinicians also worked out that their devices cost around 40% less while delivering the same level of efficacy. As a result, the team concluded that although further evaluation is required before their shielding can enter human trials, their concept could yet see end-use in the future, as a means of reducing radiotherapy’s side-effects in various different cancer patients.
“Personalized 3D printed radioprotectant devices may have great potential to reduce radiation toxicity in clinical settings,” concluded the researchers in their paper. “This personalized approach could be applicable to a variety of cancers that respond to radiation therapy, including head and neck, lung, prostate, anal, skin, and gynecological cancers, sarcomas and lymphomas.”
3D printed cancer-easing devices
By combining 3D printing and scanning technologies, it’s now easier than ever to produce patient-specific devices that ease the suffering of those undergoing cancer treatment. Scientists at the Pohang University of Science and Technology (POSTECH) have developed 3D printed esophageal stents, which are designed to ease dysphagia in radiotherapy patients.
In the future, the POSTECH team believes that their devices could be loaded with cells to treat tissue-specific inflammation or be used to address everyday injuries such as cuts or burns. In a similar vein, Adaptiiv Medical Technologies’ software is often deployed to 3D print oncological devices, that are capable of modulating radiation dosage to account for missing patient tissues.
Elsewhere, additive manufacturing is also being used by scientists at Hanyang University to create highly efficient gamma radiation detectors. During testing, the team’s novel device has demonstrated a similar decay time and intrinsic detection efficiency to a commercial scintillator, lending it potential applications in areas where rapid detection is needed.
The researchers’ findings are detailed in their paper titled “.”
The research was co-authored by James D. Byrne, Cameron C. Young, Jacqueline N. Chu, Jennifer Pursley, Mu Xian Chen, Adam J. Wentworth, Annie Feng, Ameya R. Kirtane, Kyla A. Remillard, Cindy I. Hancox, Mandar S. Bhagwat, Nicole Machado, Tiffany Hua, Siddartha M. Tamang, Joy E. Collins, Keiko Ishida, Alison Hayward, Sarah L. Becker, Samantha K. Edgington, Jonathan D. Schoenfeld, William R. Jeck, Chin Hur and Giovanni Traverso.
* This article is reprinted from 3D Printing Industry. If you are involved in infringement, please contact us to delete it.
Author: Paul Hanaphy

Leave A Comment