Researchers at the UK-based Staffordshire University have developed an ultra-low-cost insole with integrated sensing capabilities that could help prevent the growth of life-threatening foot ulcers in diabetics.
Rather than using electronic sensors to monitor ulcer development, the team’s 3D printed insoles feature tiny tunable structures, capable of reliably detecting where wearers overload their feet while walking. Using this deformation data, clinicians can potentially spot the early signs of ulcers in vulnerable patients, better managing their growth and preventing the need for life-changing amputations.
“Each year, more than 26 million people worldwide develop diabetic foot ulcers and the lifetime incidence of foot ulcers in developing countries is more than 20% among people with diabetes,” explained study co-author Professor Nachi Chockalingam. “Establishing low-cost methods to help prevent foot ulcers will reduce the global socioeconomic burden of diabetes and ultimately save lives.”
“The concept reported within this paper, with further development, has the potential to transform clinical management of foot ulcer risk across the world.”

Diabetes’ deadly side-effects
Sensory neuropathy is a lived experience for many type 2 diabetics, as the disease can progressively cause nerve damage and a loss of sensation in their legs and/or feet. As a result, many patients no longer feel pain in their extremities, meaning that they load their feet more heavily than before, triggering the onset of Diabetic Foot Ulceration (DFU).
Although DFU may initially sound trivial, it can effectively open wounds that go unnoticed and become infected, thus diabetes is now the world’s most common non-traumatic cause of amputation. In general, clinicians agree that reducing plantar pressure is vital to therapeutically managing diabetic feet, and they often prescribe footwear that’s designed to protect ulcerated areas from high loading.
Such orthotics have been in popular use for some time now, but their design is more reliant on the clinical intuition of GPs, than evidence of when diabetic foot pressures pass critical levels. Where complex shoe pressure-monitoring systems do exist, they often rely on expensive electronic sensors and cumbersome data tracking devices, which prevent their application within real-world scenarios.

As a result, the Staffordshire team has identified a need to act on the mounting evidence that pressure threshold-based devices are more likely to reduce the risk of recurrent DFU than current orthotic footwear, and proposed that 3D printing insoles with integrated sensory elements, could help identify overloaded foot areas more accurately moving forwards.
A novel low-cost insole design
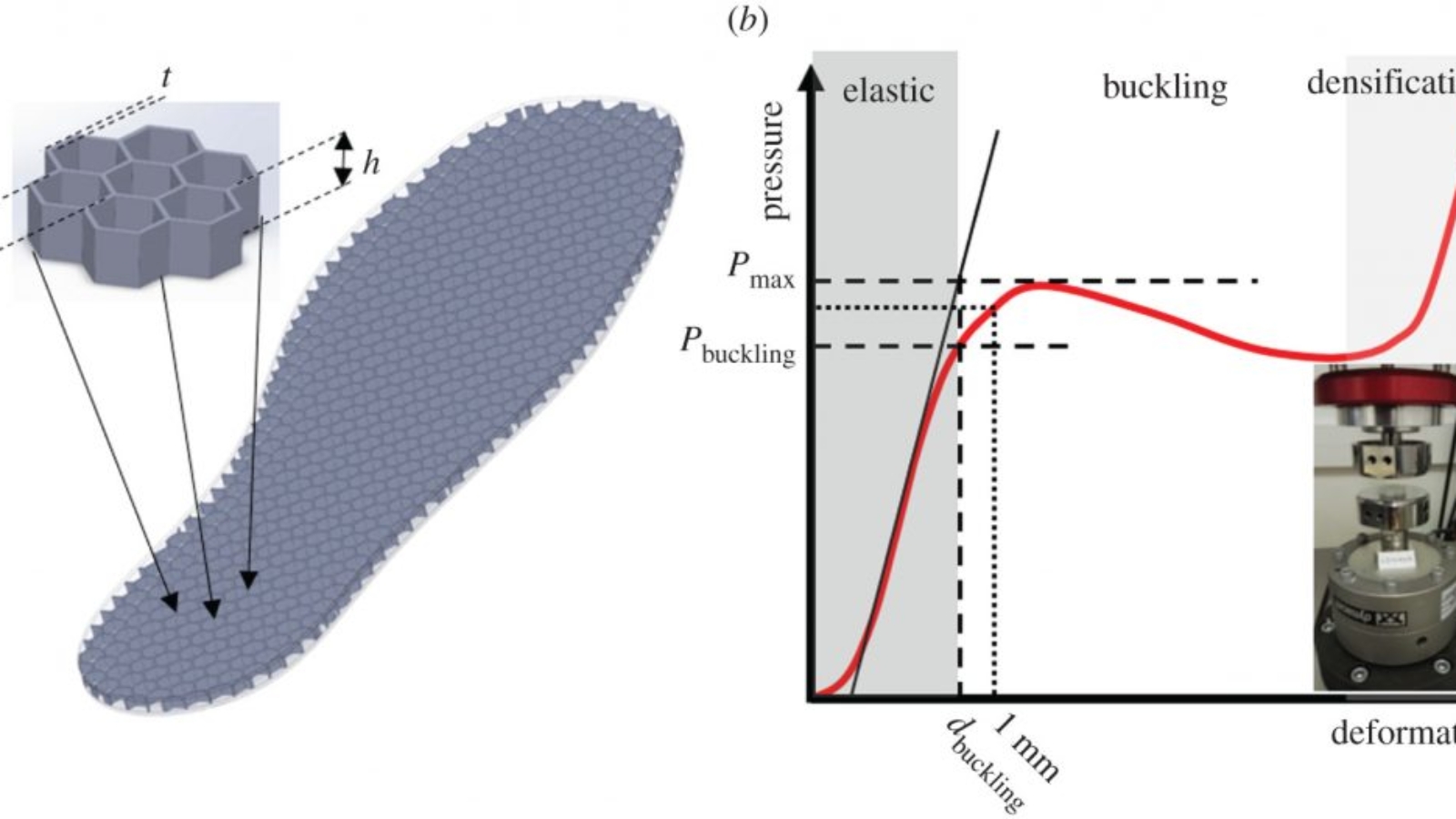
Composed of a series of tiny conjoined hexagonal structures, the team’s TPU-based insole design is highly-flexible, and features a spring-like response under low pressures. However, once loading on the device has reached a pre-programmed critical compression level, its resistance effectively drops, allowing it to shield diabetic feet from continued pressure.
After a week’s usage, the team also believe that their insole’s microstructures are likely to accumulate damage, changing their mechanical properties, and allowing them to map-out vulnerable foot areas. In order to assess the viability of their novel design, the researchers opted to FDM 3D print 26 samples with seven hexagonal structures each, before subjecting them to mechanical loading tests.
Manufacturing on Demand
Following 2,000 test cycles, in line with the average diabetic’s daily step count, the devices not only demonstrated long-term durability, but a defined pressure threshold of 252 kPa. What’s more, through later Finite Element (FE) analysis, the team found that this breaking point can be raised or lowered to meet the needs of specific applications, or even be tailored to create patient-specific insoles.
Although the researchers concluded that their design requires further development before it can be applied within clinical settings, they maintain that it proves the viability of using thin-walled structures as a sensory diagnostic tool, and their potential to “enhance ulceration risk assessment and inform the design of effective offloading interventions.”
“Our work has demonstrated a method to reliably detect overloading using a low-cost non-electronic technique,” concluded the study’s lead author Dr Panagiotis Chatzistergos. “We have used a 3D printed thin-wall structure that changes its properties when repeatedly loaded above or below a tunable threshold. We believe that this is a step change from current practice.”
Additive manufactured orthotics
The customization and design flexibility unlocked through additive manufacturing has increasingly seen the technology being used within footwear fabrication applications. Earlier this month, 3D model marketplace PROTIQ launched a 3D printing-based shoe tailoring tool that allows shoemakers to design and order bespoke orthopaedic footwear for clients.
Likewise, Bayer’s foot care subsidiary Dr. Scholl’s has previously worked with Wiivv to develop a line of customized 3D printed insoles. Now known as FitMyFoot, the firm’s technology allows users to 3D scan their feet and create personalized footwear, that’s designed to help reduce client foot pain and improve their body alignment.
In other areas, 3D printing has also been deployed to help diabetics through the creation of pain-free glucose-monitoring devices, such as the ‘e-ring’ developed at the National and Kapodistrian University of Athens. Once connected to a standard smartphone, the novel device is capable of using biomarkers to provide an ultra-precise reading on the wearer’s glucose levels.
The researchers’ findings are detailed in their paper titled “A novel concept for low-cost non-electronic detection of overloading in the foot during activities of daily living,” which was co-authored by Panagiotis E. Chatzistergos and Nachiappan Chockalingam.
* This article is reprinted from 3D Printing Industry. If you are involved in infringement, please contact us to delete it.
Author: Paul Hanaphy

Leave A Comment