Scientists at the Irish RCSI University of Medicine and Health Sciences have developed a novel bio-ink that can be 3D printed into tissues capable of fast-forwarding the human wound-healing process.
By integrating the platelet-rich plasma (PRP) that natural blood uses to mend tissues into a hydrogel, the team has been able to create unique, regenerative scaffolds, that they say are not only capable of rapidly healing wounds without leaving behind scarred tissue, but could have wider surgical applications as well.
“Existing literature suggests that while the PRP already present in our blood helps to heal wounds, scarring can still occur,” said RCSI Professor Fergal O’Brien. “By 3D printing PRP into a biomaterial scaffold, we can increase the formation of blood vessels while also avoiding the formation of scars, leading to more successful wound healing.”

“This technology can potentially be used to regenerate different tissues, therefore dramatically influencing the ever-growing regenerative medicine, 3D printing and personalised medicine markets.”
Advancing the science of healing
As the first line of defense against everyday environmental threats, our skin is actually one the largest, most important and complex organs in the human body. When these outer layers are breached by injury, our tissues are often capable of healing independently if left to their own devices, but some larger wounds can cause scarring or cells to not fully-regenerate, leading patients to suffer from chronic illness.
At present, the latter tends to be treated with wound cleaning, dressing and antibiotics, or in more extreme cases, the use of skin grafts to replace damaged tissues altogether. However, as is the way with other types of organ donation, natively-compatible healthy skin can be very difficult to find, thus grafts are rarely viable, particularly when treating large injuries.
To make such implants more readily available, scientists continue to experiment with the idea of creating wound-healing tissue-engineered scaffolds. Creating these tissues can be very expensive though, due to the recombinant growth factors required to vascularize them sufficiently for end-use, hence they’ve achieved limited success in practise.
As an alternative to using expensive, often only partially-effective proteins for tissue grafts, the RCSI team has therefore proposed utilizing naturally-occurring PRP instead. Applying patients’ platelets directly to their own skin would carry the risk of scarring, thus to get around this, the scientists have found a new way of implanting PRP by integrating it into a 3D printable hydrogel scaffold.
Printing platelet-loaded scaffolds
To make their bioengineered tissues possible, the researchers started by isolating the PRP in samples acquired from a local blood bank, before mixing it with a photoinitiator and gelatin into a novel bio-ink. Once ready, the team used an Allevi II system to extrude the material into scaffolds, which didn’t suffer any size or pore issues from the process, and degraded more slowly than pure hydrogel samples.
Having produced their first prototypes, the scientists went on to assess their rate of growth factor release over 14 days, something that would be critical in end-use applications. During these trials, the scaffolds were found to release 10% of their content as pure PRP, with their vascular endothelial growth factor (VEGF) dispersing fastest, meaning they likely vascularize more quickly than current implants.
Manufacturing on Demand
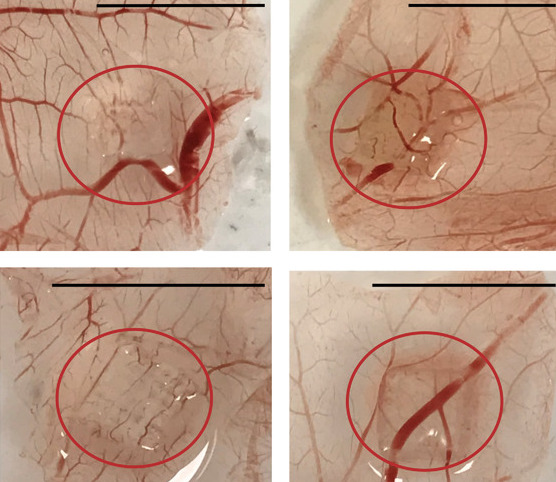
As a final test, the team then tested their wound-healing tissues by transplanting them onto chick embryos, which were incubated and cracked open for analysis. Compared to grafted control samples composed only of hydrogel, the researchers’ PRP scaffolds served to increase vascularization by a further 40%, and trigger the creation of both small blood vessels and capillaries.
As a result, although the scientists concede that their graft requires further testing to better understand host immune responses to implantation, they say their study represents a “paradigm-shifting approach for the treatment of complex wounds,” which could eventually yield a single-stage laceration-healing procedure.
“Our technology can potentially be applied to other tissue engineering applications where enhanced vascularization and the avoidance of fibrosis is desired,” concluded the team. “In addition, the use of autologous growth factors released from PRP within a 3D printed implant has great potential for clinical translation, offering several advantages over the use of recombinant growth factors.”

Bioprinting’s skin implant potential
They may not have made it to surgical theatres just yet, but 3D bioprinted tissues have come on leaps and bounds over the last year. Just last month, the NOVOPLASM consortium announced it had developed a novel way of treating infected burns and improving the wound healing of skin grafts, in which it combined bioprinting and cold plasma technology.
Earlier this year, scientists at Pennsylvania State University also came up with a means of simultaneously repairing skin and bone ailments, in which two unique bio-inks can be directly bioprinted into wound sites. Leveraging their approach, the team has already been able to quickly repair a hole in the skull and skin of a rat model during a single test procedure.
Similarly, in the skincare market, the likes of South Korean pharma firm HK inno.N have developed 3D printed skin models of their own, in order to test autoimmune and skin disorder drugs. Working with bioprinting specialist T&R Biofab, the company has unveiled plans to use its artificial tissues to conduct in-depth research into the efficacy of skin disease medications, before they hit the market.
The researchers’ findings are detailed in their paper titled “.” The research was co-authored by Rita I. R. Ibanez, Ronaldo J. F. C. do Amaral, Christopher R. Simpson, Sarah M. Casey, Rui L. Reis, Alexandra P. Marques, Ciara M. Murphy and Fergal J. O’Brien.
* This article is reprinted from 3D Printing Industry. If you are involved in infringement, please contact us to delete it.
Author: Paul Hanaphy

Leave A Comment