Researchers at Guangxi Medical University Hospital in China used 3D printing to produce custom titanium prostheses with mesh patches for five patients with distal radius giant cell tumors between 2018 and 2021. By precisely matching each patient’s anatomy, the implants improved ligament attachment, joint stability, and early wrist mobility.
Postoperative outcomes demonstrated promising results. However, complications such as distal radioulnar dislocation and ulnar impaction syndrome highlighted the critical importance of surgical precision. The study suggests that additive manufacturing could transform reconstructive bone surgery, though broader validation is needed before widespread clinical adoption.

Customized 3D Printed Implants and Surgical Approach
Traditional reconstruction methods—such as arthrodesis, autologous fibula grafts, ulnar transposition, or conventional prostheses—frequently compromise wrist function and long-term stability. In contrast, 3D printing enables the fabrication of fully customized implants that precisely conform to each patient’s anatomy.
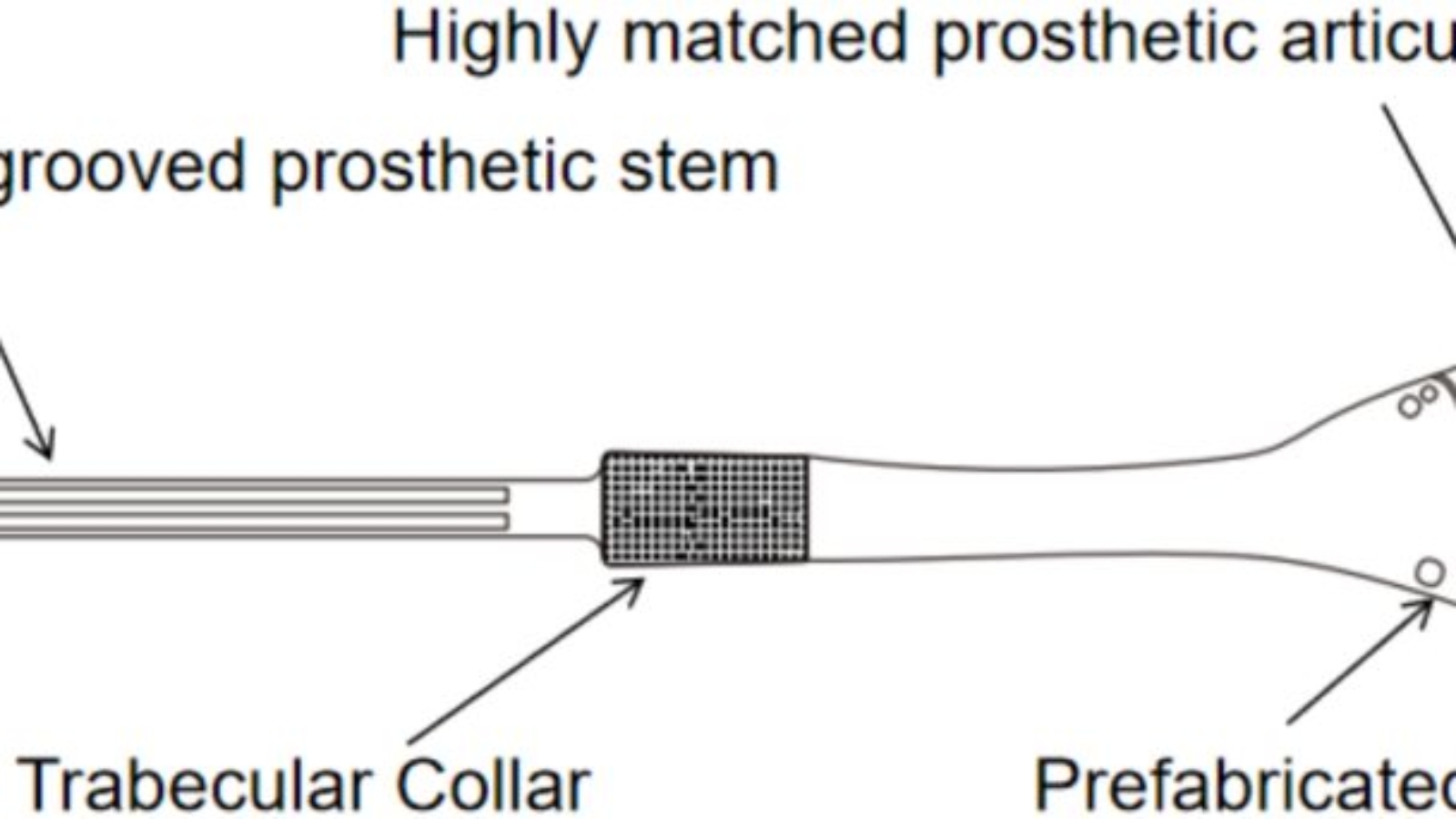
Between January 2018 and January 2021, Guangxi Medical University Hospital treated five patients with distal radial giant cell tumors using 3D printed all-metal prostheses augmented with mesh patches. During surgery, tumors were carefully excised while preserving as much of the joint capsule and surrounding ligaments as possible. The implant stem incorporated textured surfaces and grooves to optimize bone cement fixation, and the distal end faithfully replicated the natural radius with pre-fabricated holes for secure ligament and capsule attachment.
Postoperative rehabilitation commenced immediately with finger exercises, progressing to wrist flexion and extension at three weeks, and rotational movements at six weeks, supporting early functional recovery and long-term joint stability.

Functional Recovery, Limitations, and Implications
In this study, postoperative outcomes—including pain, range of motion, and grip strength—were assessed alongside oncological results, complications, and degenerative changes in the wrist joint. Functional recovery was evaluated using the Mayo wrist score system.
After an average follow-up of 40.8 months, patients demonstrated meaningful functional recovery: wrist motion averaged 20° dorsiflexion, 21.6° palmar flexion, 71.2° pronation, and 50° supination, with grip strength reaching 64% of the unaffected side. No infections or prosthesis loosening were observed. Two patients experienced distal radioulnar dislocation, and one developed ulnar impaction syndrome due to subtle misalignment, underscoring the critical importance of precise prosthesis placement and careful preservation or reconstruction of the triangular fibrocartilage complex (TFCC).
While the results show that 3D printing offers technical advantages over conventional methods, its success relies on meticulous surgical planning, accurate prosthesis alignment, and preservation or reconstruction of soft tissues. The small sample size and limited follow-up mean these results may not reflect broader patient outcomes or capture long-term issues such as joint surface degeneration, prosthesis wear, or risks of dislocation and ulnar deviation. These limitations highlight that, despite improving fit, fixation, and joint stability, the technique requires rigorous postoperative management and further validation in larger, longer-term studies.
Manufacturing on Demand

3D Printed Custom Prostheses for Optimal Fit
Additive manufacturing is increasingly being applied to complex reconstructions, where conventional prostheses often compromise fit, soft tissue integration, or functional recovery.
Companies like Croom Medical are developing 3D printed porous lattice implants that enhance bone integration and mechanical performance. Renishaw has created metal spinal implants with lattice structures that mimic bone properties, improving osseointegration compared to traditional manufacturing. Lincotek has achieved FDA clearance for 3D printed spine implants, demonstrating regulatory acceptance and clinical readiness.
These cases show that 3D printing delivers precisely matched implants, stronger soft tissue attachment, and faster functional recovery, making it a superior option for bone reconstructions. While mid-term results are promising, long-term durability and joint surface performance remain untested, so careful surgical planning and postoperative monitoring remain essential.
.
You might also like:
Create it REAL and Vitalitecs bring digital orthopedic manufacturing to Mexico: Under the agreement, Vitalitecs will operate as both a reseller of Create it REAL’s Embrace production solutions and a local 3D print service provider. This approach is intended to give orthopedic clinics and workshops flexibility in how they adopt digital manufacturing, either by bringing production in-house with training and support or by outsourcing production to a local service partner.
* This article is reprinted from 3D Printing Industry. If you are involved in infringement, please contact us to delete it.
Author: Paloma Duran

Leave A Comment