
[Image credit: Health Canada]
Creating better-fitting, longer-lasting and higher-performing bone implants is an ongoing quest for orthopaedists and surgeons alike. 3D printing is contributing enormously to the advancements in this area.
The technology is enabling implant manufacturers to create implants with enhanced functionality and more personalised to specific patient needs. Furthermore, 3D printing opens the door to personalised implants which can be created at the point of care.
This week, we continue our 3D Printing Application Spotlight series by looking at the use of 3D printing for medical implants, as well as the benefits and current applications of the technology.
The medical 3D printing market in 2019
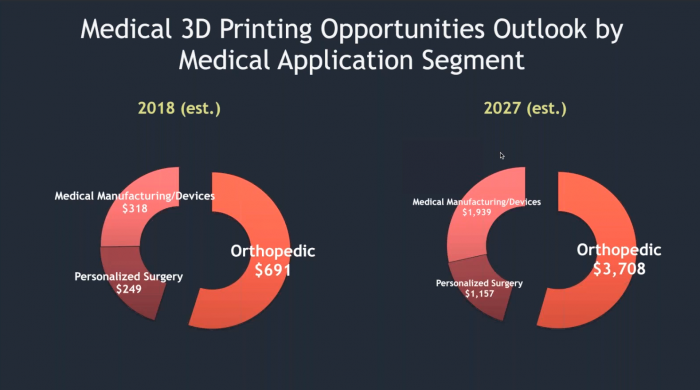
[Image credit: SmarTech Analysis]
Orthopaedic implants — medical devices used surgically to replace a missing joint or bone — are just one opportunity 3D printing offers to the medical industry.
The orthopaedics 3D printing market was valued at $691 million in 2018 and is predicted by SmarTech Analysis to grow into a $3.7 billion market by 2027.
Although implant manufacturing is a fairly new application for 3D printing — it was first used around 2007 — it has experienced rapid growth over the last decade.
In 2010, an early adopter of Arcam’s Electron Beam Melting (EBM) metal 3D printing technology received the first FDA approvals for 3D-printed implants. Seven years later, more than 300 3D printers all over the world were producing orthopaedic products.
Today, the technology is being used to create hip and knee joint replacements, cranial reconstruction implants and spinal implants. As of 2019, over 600,000 implants are estimated to be produced with the help of 3D printing. By 2027, this number is set to top 4 million.
With such a huge growth opportunity, it comes as no surprise that all of the major medical device manufacturers are increasingly embracing 3D printing technology.
Stryker, one of the largest medical technology companies in the world, has recently launched its own 3D-printed implants, including the 3D-printed Tritanium TL Curved Posterior Lumbar Cage. This hollow-bodied spinal implant received FDA approval in March 2018.
Alongside Stryker, other notable orthopaedic device manufacturers like DePuy Synthes, a subsidiary of Johnson & Johnson, and Medtronic are investing heavily into 3D printing. The latter launched a 3D printing platform, TiONIC Technology, in May 2018, with the aim of enabling more complex designs and integrated surface technologies for spinal surgical implants.
In addition to established medical device manufacturers, medical startups have also emerged over the last decade, developing proprietary approaches to 3D-printed orthopaedic implants.
Among them are companies like Osseus Fusion Systems, Nexxt Spine, 4WEB Medical and SI-BONE. Some of the products from these companies have already received FDA approval and have been used to successfully treat patients.
Clearly, there has been an upward trajectory for 3D-printed implants over the last decade. But what exactly makes this technology so useful for medical implants?
The benefits of 3D-printed implants
Design flexibility

Implants 3D printed using Arcam’s EBM technology [Image credit: Arcam]
With 3D printing, complex designs can be created that would otherwise be challenging to achieve with traditional technologies. Implant manufacturers can use this benefit to produce implants with intricate design features like trabecular structures.
Trabecular bone is one of the two types of bone tissues found in the human body. It has a spongy, porous structure that can be difficult to mimic in an implant. Traditionally, implant manufacturers use a special coating to create a trabecular structure on the implant. However, this carries a risk of the implant’s delamination and failure.
With 3D printing, on the other hand, implants with a trabecular structure can be produced directly, thus bypassing the coating process. More importantly, the trabecular, porous structure integrated into a 3D-printed implant creates a stronger implant with a reduced risk of delamination.
Such design flexibility is offered by metal 3D printing technologies like Selective Laser Melting or Electron Beam Melting. These technologies apply a powerful energy source like a laser (SLM) or an electron beam (EBM) on a thin layer of a biocompatible powder like titanium.
By repeating this process on hundreds of layers, it is possible to create a complex implant that will adapt to the human bone structure much more efficiently than traditionally made implants.
Another significant benefit of porous 3D-printed implants is improved osseointegration.
Osseointegration is a process which allows an implant to become a permanent part of the body. The porous trabecular structure allows a bone to grow inside the pores, further strengthening the bond between the implant and the existing bone.
Reduced stress shielding

A topologically-optimised hip implant [Image credit: Altair]
Furthermore, medical device manufacturers can design implants that mimic a patient’s bone stiffness and density. In addition to improving osseointegration, 3D-printed implants can reduce stress shielding and further enhance physical function.
Stress shielding refers to the phenomena by which metal implants remove typical stresses from a patient’s bone. The result is the reduction in bone density, which causes the bone to become weaker. Stress shielding can lead to fractures and dislocation. For this reason, designing an implant as close to the patient’s bone tissue as possible is key to reducing stress shielding and eliminating these unwanted effects.
In a recent example of this, IT company, Altair, combined 3D printing and topology optimisation software to create an improved hip stem implant.
By inputting parameters like size, weight and the expected load the implant would bear, topology optimisation software was used to create a new design for a hip implant. The optimised design distributes stress and strain in a more efficient way than a generic implant.
Furthermore, topology optimisation software helped to determine where the material could be replaced with lattice structures to make the implant lighter.
When tested, the optimised implant offered a stress shielding reduction of 50.7%. At the same time, its endurance limit increased to about 10 million cycles. This means that the hip implant could endure jogging from Los Angeles to New York and back — twice.
3D printing patient-specific implants
In more complex cases, off-the-shelf implants often cannot provide the necessary flexibility required. 3D printing could help in such cases, offering the ability to customise and personalise medical devices, including implants.
To produce a patient-specific implant, manufacturers use the data acquired from a patient scan, such as a computed tomography (CT) or magnetic resonance imaging (MRI) scan. The patient’s data is then imported into CAD, prepared for production, 3D printed and finished.
Using a custom, 3D-printed implant offers the potential for decreased surgical time and improved implant fit.
Currently, 3D printing can be used to create custom cranial and jaw implants where aesthetic requirements are as important as functionality.
For example, a 10 year-old Chinese boy received a 3D-printed jaw implant in 2018. He had a tumour in his jaw that could not have been removed without causing significant facial malformation.
The surgical team concluded that a conventional facial reconstruction was too dangerous for such a young patient. Looking for a better solution, they turned to 3D printing, using digital models of the boy’s jaw to design a perfectly adapted custom titanium implant.
According to the surgeons, the jaw implant was easy to fit since it was based on the patient’s anatomy. Three months after the procedure, the implantation proved successful, with the jaw being aligned well and a large amount of tissue growing.
3 examples of 3D-printed implants
A 3D-printed hip implant enables extreme mountain climbing

[Image credit: Arcam]
Romano Benet and his wife, Nives Meroi, have been summiting the world’s most dangerous mountains for many years. In 2017, the mountaineering team became the first couple to climb all 14 of the world’s highest peaks. However, achieving this feat would likely have proved impossible without the help of 3D printing.
Benet was suffering from bilateral avascular necrosis, which, essentially, leads to the bone’s collapse.
When first diagnosed, Benet and his wife were three summits shy of completing the world circuit of all 14 mountains. To continue their journey, the mountaineer needed a stable implant that would allow him to quickly recover.
For this reason, Benet’s surgeon decided to go with a 3D-printed implant.
The implant, known under the Delta Trabecular Titanium (TT) cup brand name, was produced by Italian medical device company, Lima Corporate, using Arcam’ EBM 3D printer.
By combining Lima’s Trabecular Titanium technology and 3D printing, it was possible to create implants that mimicked the porous structure of natural bone.
Thanks to this trabecular structure, a 3D-printed implant can withstand mechanical stresses during rigorous activity. Benet’s surgeon, who had implanted TT cups a handful of times on other patients, believed that in addition to offering great stability and strength, 3D-printed implants also have the potential to last beyond the lifespan of conventional implants.
When Benet received his first, non-3D-printed implant, he had suffered many months of inactivity before starting to climb again. With a 3D-printed implant, the mountaineer was able to resume his activity after two and a half months.
Ultimately, the 3D-printed implant did its job: it enabled Benet to quickly recover and successfully complete his quest of reaching the last three high-altitude peaks.
Osseus Fusion Systems: On the way towards personalised metal implants
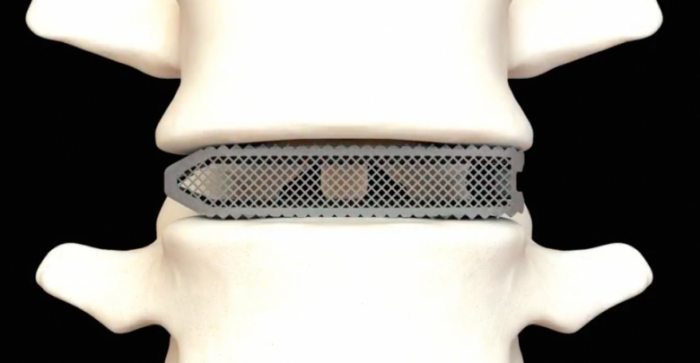
Osseus’ Aries titanium spinal implant [Image credit: Osseus]
Founded in 2012, Osseus Fusion Systems is a US-based company with a focus on developing advanced medical products for spinal-related injuries.
To improve the quality and functionality of its products, Osseus has developed a proprietary 3D printing technology called PL3XUS.
The technology is based on powder bed fusion 3D printing, specifically Selective Laser Melting (SLM), and can create 80% porous titanium implants, optimised for bone fusion and biological fixation (the process whereby a living bone attaches permanently to the implant surface).
In August 2018, Osseus achieved FDA 510(k) clearance for Aries, its family of additively manufactured lumbar interbody fusion devices. The Aries family of implants is designed to help surgeons ease back pain and reduce spinal recovery time.
Earlier this year, Osseus’ Aries product has, for the first time, been put into practice by Joseph Spine, a centre for spine and scoliosis surgery. PL3XUS technology made it possible to design the implant with a similar architecture to the bone of a patient, facilitating the bone’s in-growth.
In the next couple of years, Osseus plans to launch personalised devices based on patient’s CT Scans, X-Rays and MRIs.
With this next step, the company looks to empower hospitals to provide superior patient care and, ultimately, further improve surgery outcomes for patients.
3D printing implants with high-performance thermoplastics

An OXPEKK SLS 3D printed cranial implant [Image credit: Oxford Performance Materials]
In addition to titanium and other biocompatible metals, 3D printing can be coupled with polymers like PEEK and PEKK to produce implants. These thermoplastics are known for their high strength and biocompatibility, and also offer a few benefits over metal implants like lower costs and radiolucency.
In 2013, Oxford Performance Materials (OPM) became the first company to receive FDA clearance for a patient-specific 3D-printed PEKK cranial implant. By 2017, OPM had shipped over 1400 cranial implants and received FDA clearances for two other devices: maxillofacial and spinal implants.
The company uses Selective Laser Sintering technology, which powers OPM’s proprietary OsteoFab® platform for implant development and production. In one example, this platform enabled a patient-specific cranial implant to be designed, manufactured, tested and shipped from OPM in just 3 business days. In less than a week, surgeons successfully performed the surgery, without making any cutting or drilling modifications to reshape the implant.
3D printing for medical implants: Making an impact
Biocompatibility, load-bearing capacity and durability are the fundamental requirements for orthopaedic implants. 3D printing fully meets these requirements whilst advancing the functionality and fit of implants.
This can primarily be attributed to the ability of the technology to create complex shapes like porous structures, which help a patient’s body to adapt to an implant faster and with fewer complications.
Going forward, 3D printing for implants will continue to evolve. One particularly exciting area of ongoing research is the combination of 3D-printed implants and sensors. By developing sensor-powered implants, healthcare providers can potentially improve patient outcomes significantly.
Inbuilt sensors could collect data like temperature around the implant, movement and strain that is being exerted on the implant. This will enable surgeons to react to any potential issues early on and to tailor treatment to the needs of individual patients.
Renishaw, a UK manufacturer of metal 3D printers, and Western University have already set up the Additive Design in Surgical Solutions (ADEISS) Centre on the university’s campus. The centre brings together academics and clinicians to work on developing novel 3D-printed medical devices like those described above.
Clearly, 3D printing technology is gaining a strong foothold within the orthopaedics segment.
However, the technology will need to mature to truly unlock its potential for custom-created implants produced at the point of care.
Admittedly, only a small percentage of implants are currently custom-created with 3D printing. While the technology holds huge potential, questions around standardisation and regulation still need to be addressed.
That said, creating custom medical implants is where the technology could make the biggest impact and enable more people to benefit from personalised healthcare. We believe this direction will see significant traction in the years to come.
In our next article, we’ll be taking a look at how 3D printing can enhance rocket manufacturing. Stay tuned!